9 0 6 7 6
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

Th1/Th17 细胞因子谱与 COPD 患者的疾病严重程度和恶化频率相关
Authors Yu Y, Zhao L, Xie Y, Xu Y, Jiao W, Wu J, Deng X, Fang G, Xue Q, Zheng Y, Gao Z
Received 2 March 2020
Accepted for publication 11 May 2020
Published 8 June 2020 Volume 2020:15 Pages 1287—1299
DOI https://doi.org/10.2147/COPD.S252097
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Chunxue Bai
Background: T helper (Th) cell cytokine imbalances have been associated with the pathophysiology of chronic obstructive pulmonary disease (COPD), including the Th1/Th2 and Th17/T regulatory cells (Treg) paradigms. Clarifying cytokine profiles during COPD acute exacerbation (AE) and their relationships with clinical manifestations would help in understanding the pathogenesis of disease and improve clinical management.
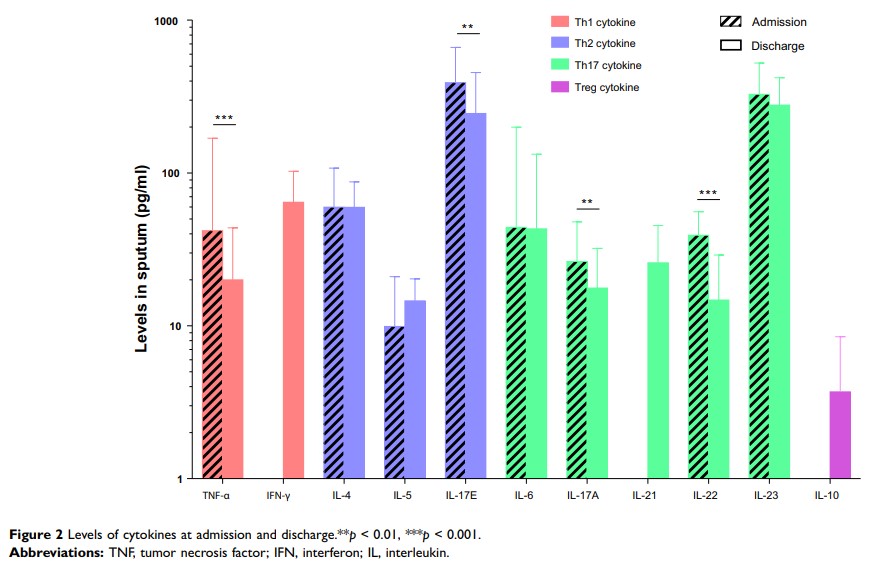
Materials and Methods: Eighty seven patients admitted to the hospital with AEs of COPD were included in this study, and follow-up was conducted after discharge (every 30 days, for a total of 120 days). Sputum samples of patients at different time points (including at admission, discharge, and follow-up) were collected, and sputum cytokine profiling (12 cytokines in total) was performed using a Luminex assay.
Results: According to the cytokine profiles at admission, patients were divided into three clusters by a k-means clustering algorithm, namely, Th1high Th17high (n=26), Th1lowTh17low (n=56), and Th1high Th17low (n=5), which revealed distinct clinical characteristics. Patients with Th1high Th17low profile had a significantly longer length of non-invasive ventilation time and length of hospital stay than patients with Th1high Th17high profile (7 vs 0 days, 22 vs 11 days, respectively, p < 0.05), and had the highest AE frequency. Sputum levels of Th17 cytokines (IL-17A, IL-22, and IL-23) during AE were negatively correlated with AE frequency in the last 12 months (r = − 0.258, − 0.289 and − 0.216, respectively, p < 0.05). Moreover, decreased sputum IL-17A levels were independently associated with increased AE frequency, with an OR (95% CI) of 0.975 (0.958– 0.993) and p = 0.006.
Conclusion: Th1/Th17 imbalance during AE is associated with the severity of COPD. Decreased Th17 cytokine expression is correlated with increased AE frequency. The Th1/Th17 balance may be a specific target for the therapeutic manipulation of COPD.
Keywords: chronic obstructive pulmonary disease, acute exacerbation, Th1 cytokines, Th17 cytokines, therapeutic