9 0 4 9 6
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

已发表论文
在伊立替康为基础的治疗方案作为转移性结直肠癌治疗中 UGT1A1 的基因多态性的临床意义
Authors Li MM, Wang ZH, Guo J, Liu J, Li CZ, Liu L, Shi H, Liu LY, Li HH, Xie C, Zhang X, Sun WW, Fang S, Bi X
Published Date September 2014 Volume 2014:7 Pages 1653—1661
DOI http://dx.doi.org/10.2147/OTT.S67867
Received 16 May 2014, Accepted 16 July 2014, Published 23 September 2014
Purpose: The primary aim of this research was to investigate the association between uridine diphosphate glucuronosyltransferase (UGT)1A1 gene polymorphisms and the toxicities of irinotecan-based regimens in Chinese patients with metastatic colorectal cancer.
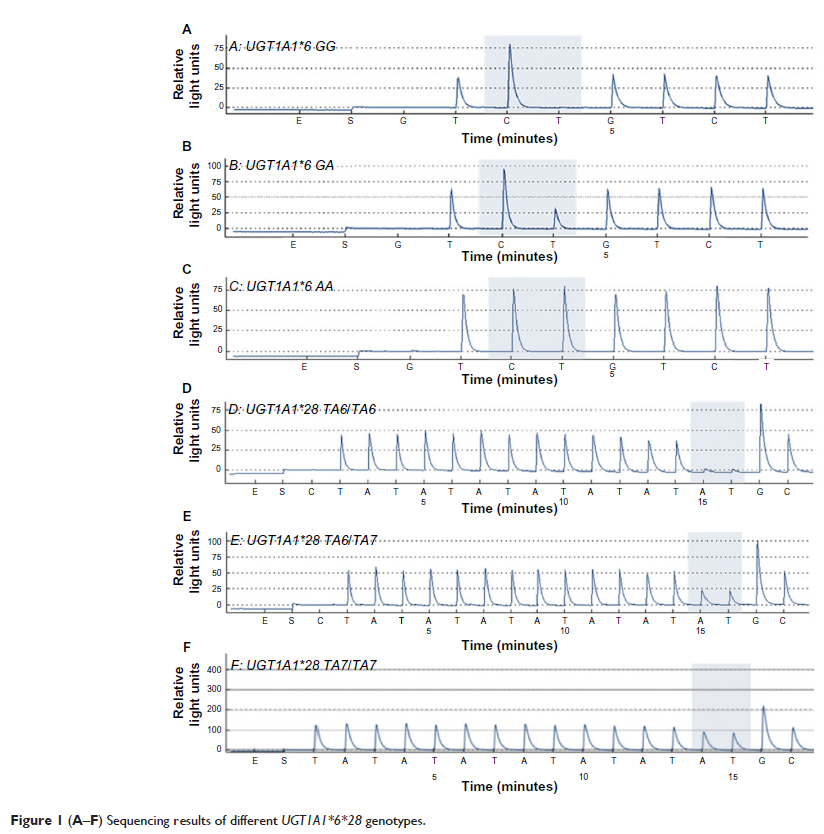
Methods: The study analyzed the distribution of UGT1A1*28/*6 gene polymorphisms by polymerase chain reaction amplification and pyrosequencing. The adverse reactions and tumor response were evaluated according to National Cancer Institute Common Toxicity Criteria for Adverse Events, Version 3.0, and Response Evaluation Criteria In Solid Tumors, Version 1.0, criteria, respectively. The correlation between UGT1A1 gene polymorphisms and severe delayed diarrhea or neutropenia was analyzed. The influences of UGT1A1*6/*28 polymorphisms on response rate and progression-free survival were also analyzed. Survival analysis was performed by the Kaplan–Meier method, and we used the log-rank test to analyze the effect of genotypes on progression-free survival, the logistic regression model for multivariate analysis, and the Cox regression model for multivariate survival analysis.
Results: A total of 167 patients with metastatic colorectal cancer who were treated with irinotecan-based regimens and with detected UGT1A1 gene polymorphisms were enrolled in this research. The rate of UGT1A1*28 homozygous wild-type TA6/6, heterozygous mutant-type TA6/7, and homozygous mutant-type TA7/7 was 65.3% (109/167), 32.3% (54/167), and 2.4% (4/167), respectively; the incidence of UGT1A1*6 wild-type G/G was 67.1% (112/167), heterozygous mutant-type G/A accounted for 28.7% (48/167), and seven cases were homozygous mutant-type A/A (4.2%; 7/167). The incidence of grade 3 or 4 delayed diarrhea in patients carrying UGT1A1*6 (G/A and A/A) was higher than that in the wild-type (G/G) (P =0.021). The rate was significantly lower in patients with the UGT1A1*28 TA6/6 wide-type genotype than those with TA6/7 and TA7/7 mutant-type genotypes (P =0.027). However, neither UGT1A1*6 (P =0.34) nor UGT1A1*28 (P =0.232) variants were significantly associated with severe neutropenia. Our study found no significant differences of severe neutropenia in patients with different numbers of mutational alleles (P =0.354), but patients with two alleles or single allele variants had more chances to develop severe diarrhea than patients with wild-type (P =0.027). No significant differences of either response rate or progression-free survival were found among different genotypes (P >0.05).
Conclusion: For irinotecan-based regimens in metastatic colorectal cancer, the UGT1A1*28 andUGT1A1*6 locus mutations can be regarded as predictors for irinotecan-associated severe delayed diarrhea, whereas no association between UGT1A1 gene polymorphisms and severe neutropenia was observed. We also found that neither clinical response nor prognosis were significantly associated with UGT1A1 gene polymorphisms.
Keywords: uridine diphosphate glucuronosyltransferase 1A1 , gene polymorphism, metastatic colorectal cancer, irinotecan
Methods: The study analyzed the distribution of UGT1A1*28/*6 gene polymorphisms by polymerase chain reaction amplification and pyrosequencing. The adverse reactions and tumor response were evaluated according to National Cancer Institute Common Toxicity Criteria for Adverse Events, Version 3.0, and Response Evaluation Criteria In Solid Tumors, Version 1.0, criteria, respectively. The correlation between UGT1A1 gene polymorphisms and severe delayed diarrhea or neutropenia was analyzed. The influences of UGT1A1*6/*28 polymorphisms on response rate and progression-free survival were also analyzed. Survival analysis was performed by the Kaplan–Meier method, and we used the log-rank test to analyze the effect of genotypes on progression-free survival, the logistic regression model for multivariate analysis, and the Cox regression model for multivariate survival analysis.
Results: A total of 167 patients with metastatic colorectal cancer who were treated with irinotecan-based regimens and with detected UGT1A1 gene polymorphisms were enrolled in this research. The rate of UGT1A1*28 homozygous wild-type TA6/6, heterozygous mutant-type TA6/7, and homozygous mutant-type TA7/7 was 65.3% (109/167), 32.3% (54/167), and 2.4% (4/167), respectively; the incidence of UGT1A1*6 wild-type G/G was 67.1% (112/167), heterozygous mutant-type G/A accounted for 28.7% (48/167), and seven cases were homozygous mutant-type A/A (4.2%; 7/167). The incidence of grade 3 or 4 delayed diarrhea in patients carrying UGT1A1*6 (G/A and A/A) was higher than that in the wild-type (G/G) (P =0.021). The rate was significantly lower in patients with the UGT1A1*28 TA6/6 wide-type genotype than those with TA6/7 and TA7/7 mutant-type genotypes (P =0.027). However, neither UGT1A1*6 (P =0.34) nor UGT1A1*28 (P =0.232) variants were significantly associated with severe neutropenia. Our study found no significant differences of severe neutropenia in patients with different numbers of mutational alleles (P =0.354), but patients with two alleles or single allele variants had more chances to develop severe diarrhea than patients with wild-type (P =0.027). No significant differences of either response rate or progression-free survival were found among different genotypes (P >0.05).
Conclusion: For irinotecan-based regimens in metastatic colorectal cancer, the UGT1A1*28 andUGT1A1*6 locus mutations can be regarded as predictors for irinotecan-associated severe delayed diarrhea, whereas no association between UGT1A1 gene polymorphisms and severe neutropenia was observed. We also found that neither clinical response nor prognosis were significantly associated with UGT1A1 gene polymorphisms.
Keywords: uridine diphosphate glucuronosyltransferase 1A1 , gene polymorphism, metastatic colorectal cancer, irinotecan