9 0 5 7 8
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

Factors influencing adherence to psychopharmacological medications in psychiatric patients: a structural equation modeling approach
Authors De las Cuevas C, de Leon J, Peñate W, Betancort M
Received 30 January 2017
Accepted for publication 28 February 2017
Published 28 March 2017 Volume 2017:11 Pages 681—690
DOI https://doi.org/10.2147/PPA.S133513
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
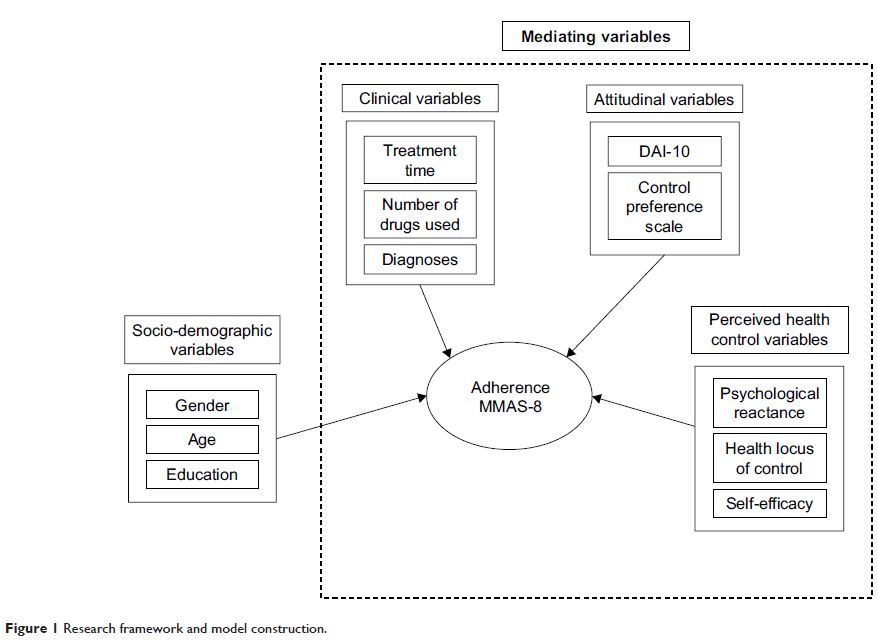
Purpose: To evaluate pathways through which sociodemographic, clinical,
attitudinal, and perceived health control variables impact psychiatric
patients’ adherence to psychopharmacological medications.
Method: A sample of 966 consecutive psychiatric outpatients was studied. The
variables were sociodemographic (age, gender, and education), clinical
(diagnoses, drug treatment, and treatment duration), attitudinal (attitudes
toward psychopharmacological medication and preferences regarding participation
in decision-making), perception of control over health (health locus of
control, self-efficacy, and psychological reactance), and level of adherence to
psychopharmacological medications. Structural equation modeling was applied to
examine the nonstraightforward relationships and the interactive effects among
the analyzed variables.
Results: Structural equation modeling demonstrated that psychiatric patients’
treatment adherence was associated: 1) negatively with cognitive psychological
reactance (adherence decreased as cognitive psychological reactance increased),
2) positively with patients’ trust in their psychiatrists (doctors’ subscale),
3) negatively with patients’ belief that they are in control of their mental
health and that their mental health depends on their own actions (internal subscale),
and 4) positively (although weakly) with age. Self-efficacy indirectly
influenced treatment adherence through internal health locus of control.
Conclusion: This study provides support for the hypothesis that perceived health
control variables play a relevant role in psychiatric patients’ adherence to
psychopharmacological medications. The findings highlight the importance of
considering prospective studies of patients’ psychological reactance and health
locus of control as they may be clinically relevant factors contributing to
adherence to psychopharmacological medications.
Keywords: attitude to health, medication adherence, health behavior,
internal-external control, model, statistical, psychiatry