9 0 5 7 8
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

已发表论文
以超声波定向毁灭基质细胞衍生因子-1 的微泡载体令糖尿病肾病大鼠体内间充质干细胞导向肾脏
Authors Wu S, Li L, Wang G, Shen W, Xu Y, Liu Z, Zhuo Z, Xia H, Gao Y, Tan K
Published Date December 2014 Volume 2014:9(1) Pages 5639—5651
DOI http://dx.doi.org/10.2147/IJN.S73950
Received 8 September 2014, Accepted 25 October 2014, Published 3 December 2014
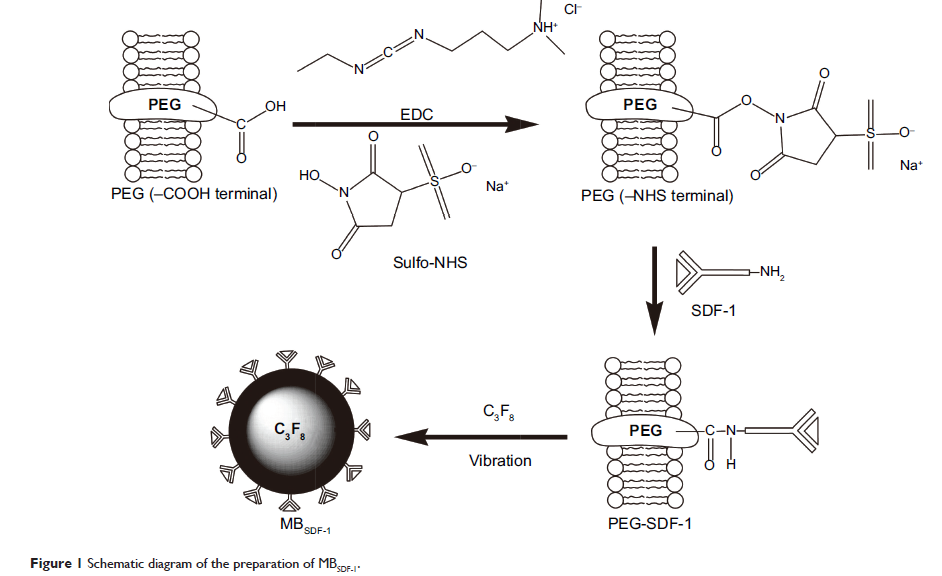
Abstract: Mesenchymal stem cell (MSC) therapy has been considered a promising
strategy to cure diabetic nephropathy (DN). However, insufficient MSCs can
settle in injured kidneys, which constitute one of the major barriers to the
effective implementation of MSC therapy. Stromal cell-derived factor-1 (SDF-1)
plays a vital role in MSC migration and involves activation, mobilization,
homing, and retention, which are presumably related to the poor homing in DN
therapy. Ultrasound-targeted microbubble destruction has become one of the most
promising strategies for the targeted delivery of drugs and genes. To improve
MSC homing to DN kidneys, we present a strategy to increase SDF-1 via
ultrasound-targeted microbubble destruction. In this study, we developed
SDF-1-loaded microbubbles (MBSDF-1) via covalent conjugation. The
characterization and bioactivity of MBSDF-1 were assessed in vitro.
Target release in the targeted kidneys was triggered with diagnostic ultrasound
in combination with MBSDF-1. The related bioeffects were also
elucidated. Early DN was induced in rats with streptozotocin. Green fluorescent
protein-labeled MSCs were transplanted intravenously following the target
release of SDF-1 in the kidneys of normal and DN rats. The homing efficacy was
assessed by detecting the implanted exogenous MSCs at 24 hours. The in
vitro results showed an impressive SDF-1 loading efficacy of 79% and a loading
content of 15.8 µg/mL. MBSDF-1 remained bioactive as a
chemoattractant. In the in vivo study, SDF-1 was successfully released in the
targeted kidneys. The homing efficacy of MSCs to DN kidneys after the target
release of SDF-1 was remarkably ameliorated at 24 hours compared with
control treatments in normal rats and DN rats. In conclusion,
ultrasound-targeted MBSDF-1 destruction could promote the homing of
MSCs to early DN kidneys and provide a novel potential therapeutic approach
for DN kidney repair.
Keywords: mesenchymal stem cell, ultrasound, microbubbles, homing, stromal cell-derived factor-1, diabetic nephropathy
Keywords: mesenchymal stem cell, ultrasound, microbubbles, homing, stromal cell-derived factor-1, diabetic nephropathy