9 0 5 7 8
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

铜绿假单胞菌感染的支气管扩张患者对抗生素耐药:患病率,危险因素和预后影响
Authors Gao YH, Guan WJ, Zhu YN, Chen RC, Zhang GJ
Received 29 August 2017
Accepted for publication 28 November 2017
Published 9 January 2018 Volume 2018:13 Pages 237—246
DOI https://doi.org/10.2147/COPD.S150250
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Charles Downs
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Chunxue Bai
Background and
aims: Pseudomonas aeruginosa (PA)
is the most common pathogen in bronchiectasis and frequently develops
resistance to multiple classes of antibiotics, but little is known about the
clinical impacts of PA-resistant (PA-R) isolates on bronchiectasis. We,
therefore, investigated the prevalence, risk factors and prognostic
implications of PA-R isolates in hospitalized bronchiectasis patients.
Patients and methods: Between June 2011 and July 2016, data from adult
bronchiectasis patients isolated with PA at the First Affiliated Hospital of
Zhengzhou University were retrospectively analyzed. PA was classified as PA-R
in case antibiogram demonstrated resistance on at least one occasion.
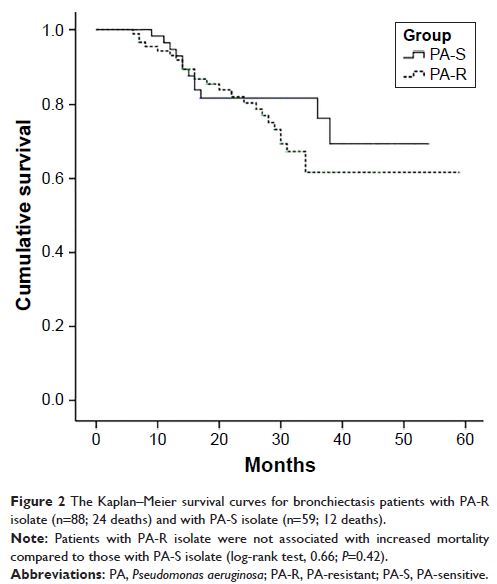
Results: Seven hundred forty-seven bronchiectasis
patients were assessed. Of these, 147 (19.7%) had PA isolate in the sputum or
bronchoscopic culture. PA-R and PA-sensitive accounted for 88 (59.9%) and 59
(31.1%) patients, respectively. In multivariate model, factors associated with
PA-R isolate in bronchiectasis included prior exposure to antibiotics (odds
ratio [OR] =6.18), three or more exacerbations in the previous year (OR =2.81),
higher modified Medical Research Council dyspnea scores (OR =1.93) and greater
radiologic severity (OR =1.15). During follow-up (median: 26 months;
interquartile range: 6–59 months), 36 patients died, of whom 24 (66.7%) had
PA-R isolate at baseline. However, PA-R isolate was not associated with greater
all-cause mortality in bronchiectasis.
Conclusion: PA-R infection is common among bronchiectasis
patients, mainly determined by prior exposure to antibiotics, frequent
exacerbations, more pronounced dyspnea and more severe radiologic involvement.
However, PA-R isolate is not an independent risk factor for all-cause mortality
in bronchiectasis.
Keywords: bronchiectasis,
antibiotic resistance, Pseudomonas aeruginosa ,
risk factors, mortality