9 0 6 7 6
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

妊娠合并或不合并狼疮性肾炎的治疗和结果:系统综述和荟萃分析
Authors Wu JY, Ma JH, Zhang WH, Di W
Received 24 December 2017
Accepted for publication 21 March 2018
Published 11 May 2018 Volume 2018:14 Pages 885—901
DOI https://doi.org/10.2147/TCRM.S160760
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Background: Although it is well established that systemic lupus erythematosus
(SLE) negatively affects pregnancy outcomes, there is insufficient evidence on
the effect of lupus nephritis (LN) on antenatal management and pregnancy
outcomes. We performed a systematic review and meta-analysis to determine the
association of LN with management and pregnancy outcomes in SLE patients.
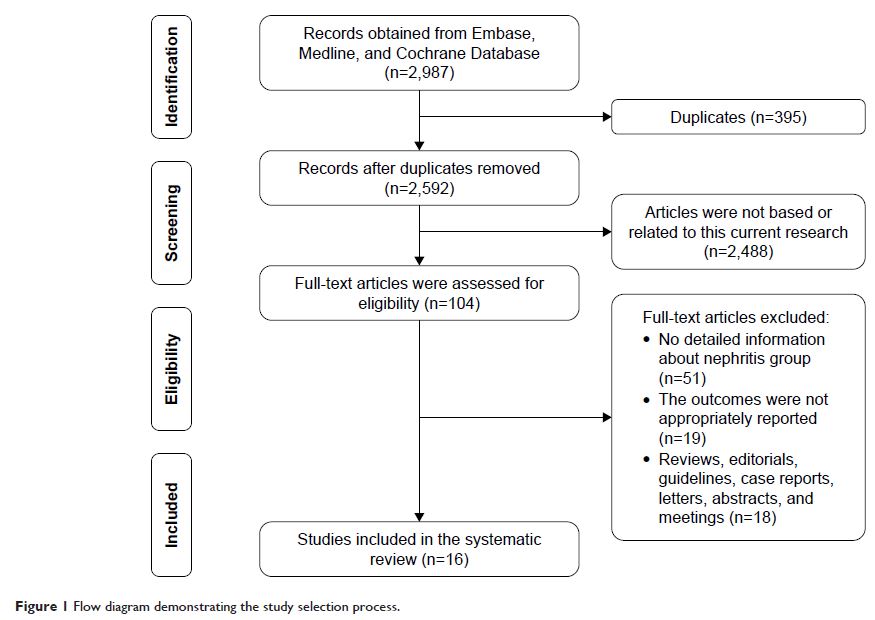
Methods: Embase, Medline, Cochrane, and
ClinicalTrials.gov were carefully searched for relevant English and Chinese
language studies. A total of 2,987 articles were reviewed. Data were extracted
that compared management and pregnancy outcomes in SLE pregnant women with LN
vs without LN. Risk of bias was assessed by a modified version of the
Newcastle-Ottawa Scale and the STROBE checklist. Combined odds ratios (OR) and
95% confidence intervals (CI) were obtained and sensitivity analysis was
performed using RevMan 5.3 software.
Results: Sixteen studies, including 1,760 pregnant patients
with SLE, were included. Gestational hypertension (OR=5.65, 95% CI=2.94–10.84),
preeclampsia (OR=2.84, 95% CI=1.87–4.30), SLE flare (OR=2.66, 95%
CI=1.51–4.70), renal flare (OR=15.18, 95% CI=5.89–39.14), proteinuria (OR=8.86,
95% CI=4.75–16.52), and hypocomplementemia (OR=2.86, 95% CI=1.68–4.87) were
significantly affected in pregnant women with LN. Anti-Sjögren’s
syndrome-related antigen A/Ro autoantibodies were negatively associated with
pregnant women with LN (OR=0.57, 95% CI=0.33–0.98). Pregnant women with LN
presented a significant decrease in live births (OR=0.62, 95% CI=0.49–0.80) and
a significant increase in preterm births (OR=1.92, 95% CI=1.49–2.49) and fetal
growth restriction (OR=1.43, 95% CI=1.08–1.91). Regarding antenatal management,
steroids (OR=2.48, 95% CI=1.59–3.87) and immunosuppressant treatment (OR=6.77,
95% CI=3.30–13.89) were more frequently used in women with LN.
Conclusion: This review identified a significant association
between the aforementioned outcomes and SLE pregnant patients with LN. In
patients with SLE, LN increased the risks for adverse pregnancy outcomes and
the use of medication. Therefore, special treatment and close monitoring should
be allocated to pregnant women with LN.
Keywords: systemic lupus
erythematosus, lupus nephritis, maternal outcomes, fetal outcomes, antenatal
management