9 0 5 7 8
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

术前负荷剂量替卡格雷和氯吡格雷对 ST 段抬高心肌梗死患者接受直接经皮冠状动脉介入治疗时无复流现象的影响:系统综述和荟萃分析
Authors Dai W, Ye Z, Li L, Su Q
Received 13 February 2018
Accepted for publication 2 May 2018
Published 4 July 2018 Volume 2018:12 Pages 2039—2049
DOI https://doi.org/10.2147/DDDT.S165431
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 3
Editor who approved publication: Dr Anastasios Lymperopoulos
Background: Previous studies have shown that ticagrelor is more effective than
clopidogrel in platelet inhibition. However, this conclusion remains
controversial. Therefore, we performed this meta-analysis to assess the effect
of preoperative loading dose ticagrelor and clopidogrel on no-reflow (NRF)
during intervention in patients with ST-segment elevation myocardial infarction
undergoing primary percutaneous coronary intervention (PPCI).
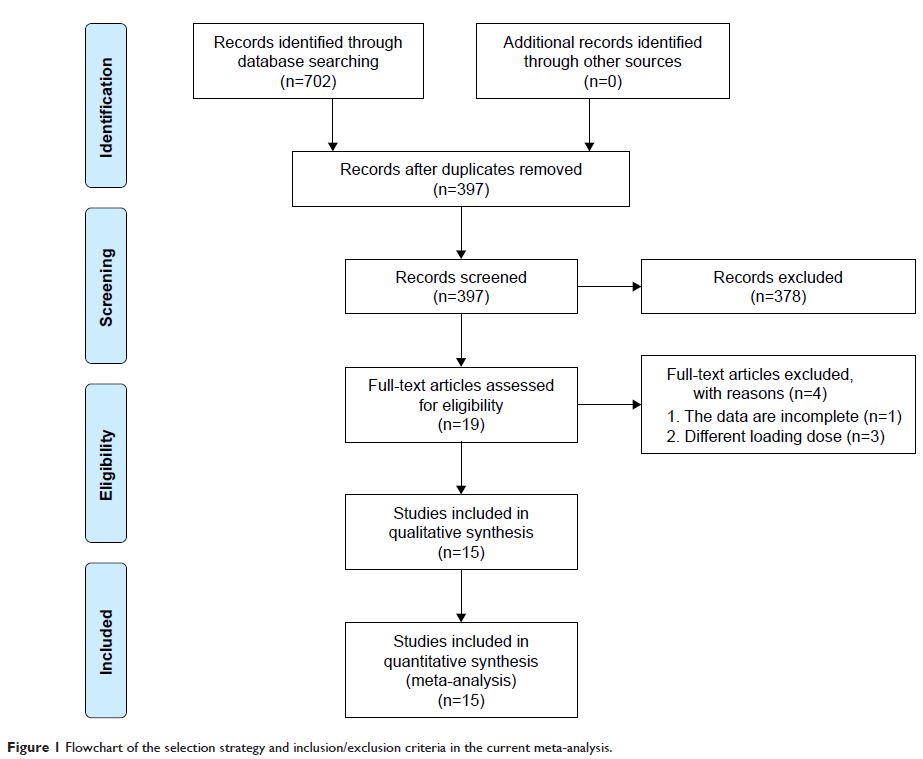
Materials and methods: Randomized controlled trials and observational
studies were reviewed. The retrieval time was limited from inception to October
1, 2017. The retrieved databases included PubMed, Embase, the Cochrane Library,
Web of Science, CBM, CNKI, the VIP database, and the Wang Fang database. RevMan
5.3 software was used for data analysis.
Results: Fourteen randomized controlled trials and one
observational study, including 4,162 patients, were included. In these
articles, 1,521 patients were in the ticagrelor group (180 mg) and 2,641
patients were in the clopidogrel group (600 mg). The meta-analysis showed that
compared with clopidogrel group, preoperative loading dose ticagrelor: 1)
significantly reduced the incidence of NRF during PPCI (95% confidence interval
[CI]: 0.15, 0.39, P <0.05) as well
as the level of postoperative corrected thrombolysis in myocardial infarction
frame count (95% CI: -8.89, -6.91, P <0.05);
2) significantly reduced the incidence of major adverse cardiovascular events
during hospitalization, including 30 and 180 days after PPCI (95% CI: 0.41,
0.82, P <0.05; 95% CI: 0.15,
0.46, P <0.05, respectively); and 3)
significantly improved thrombolysis in myocardial infarction flow after PPCI
(95% CI: 1.40, 2.45, P <0.05). No
significant difference was observed in terms of bleeding events within 30 and
180 days after PPCI (95% CI: 0.71, 1.54, P =0.82; 95%
CI: 0.81, 3.19, P =0.18,
respectively).
Conclusion: Compared with clopidogrel, loading dose
ticagrelor effectively reduced both the occurrence of NRF during PPCI and the
incidence of major adverse cardiovascular event in patients with ST-segment
elevation myocardial infarction undergoing PPCI. Furthermore, it did not
increase the risk of bleeding after PPCI.
Keywords: ticagrelor,
clopidogrel, primary PCI, no-reflow, meta-analysis