9 0 6 7 6
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

患者自控硬膜外镇痛与患者自控静脉镇痛对胃癌切除术后疼痛的控制和短期预后的影响:对 2010-2015 年间连续 3,042 例患者进行回顾性分析
Authors Wang LP, Li X, Chen H, Liang J, Wang Y
Received 21 March 2018
Accepted for publication 11 July 2018
Published 5 September 2018 Volume 2018:11 Pages 1743—1749
DOI https://doi.org/10.2147/JPR.S168892
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 5
Editor who approved publication: Dr Michael Schatman
Background: Effective postoperative analgesia is essential for rehabilitation after surgery. Many studies have compared different methods of postoperative pain management for open abdominal surgery. However, the conclusions were inconsistent and controversial. In addition, few studies have focused on gastric cancer (GC) resection. This study aimed to determine the effects of patient-controlled epidural analgesia (PCEA) on postoperative pain management and short-term recovery after GC resection compared with those of patient-controlled intravenous analgesia (PCIA).
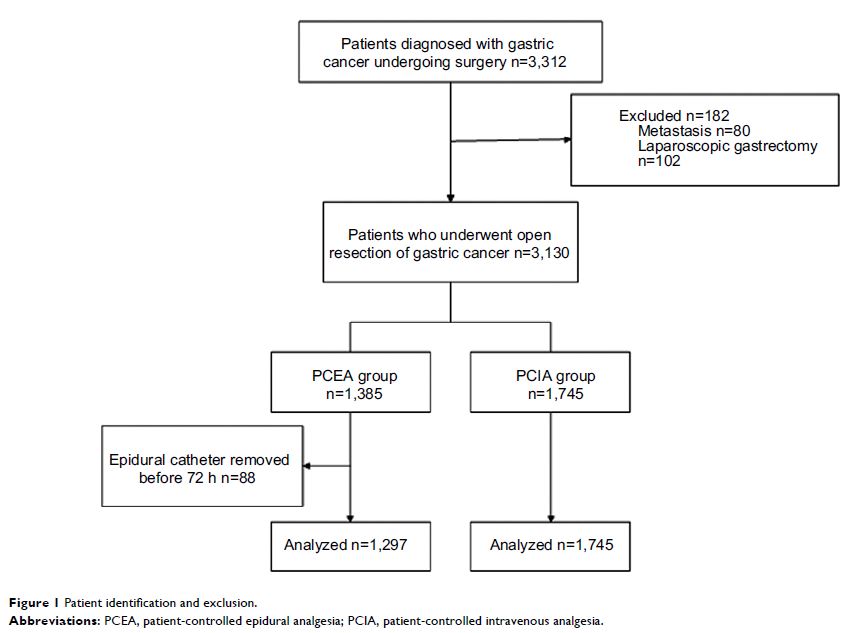
Methods: We analyzed retrospectively collected data on patients with non-metastatic GC diagnosed between 2010 and 2015 who underwent resection in a university hospital. PCIA and PCEA documented by the acute pain service team were retrospectively analyzed. A propensity score-matched analysis that incorporated preoperative variables was used to compare the short-term outcomes between the PCIA and PCEA groups.
Results: In total, 3,042 patients were identified for analysis. Propensity score matching resulted in 917 patients in each group. The PCEA group exhibited lower pain scores in the recovery room and on the first and second postoperative days (P =0.0005, P =0.0065, and P =0.0034 respectively). The time to the first passage of flatus after surgery was shorter in the PCEA group than in the PCIA group (P =0.032). The length of the hospital stay was 12.6±7.2 and 11.8±6.6 days in the PCEA and PCIA groups, respectively. No significant differences were observed in the length of hospital stay or the incidence of complications after surgery.
Conclusion: PCEA provided more effective postoperative pain management and a shorter time to the first passage of flatus than PCIA after GC resection. However, it did not have an effect on the length of hospital stay or the incidence of postoperative complications.
Keywords: gastrectomy, gastric cancer, patient-controlled analgesia, epidural analgesia, short-term outcomes, pain treatment, analgesia-related complications