9 0 5 7 8
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

微创 McKeown 和 Ivor-Lewis 食管切除术治疗食管癌或交界癌的短期疗效比较:系统综述和荟萃分析
Authors Deng J, Su Q, Ren Z, Wen J, Xue Z, Zhang L, Chu X
Received 29 March 2018
Accepted for publication 11 July 2018
Published 20 September 2018 Volume 2018:11 Pages 6057—6069
DOI https://doi.org/10.2147/OTT.S169488
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Carlos E Vigil
Purpose: Minimally invasive esophagectomy is increasingly performed for
esophageal or gastroesophageal junctional cancer, with advantages of improved
perioperative outcomes in comparison with open esophagectomy. McKeown and Ivor
Lewis are widely used procedures of minimally invasive esophagectomy, and there
have been controversies on which one is preferred for patients with resectable
esophageal or junctional cancer.
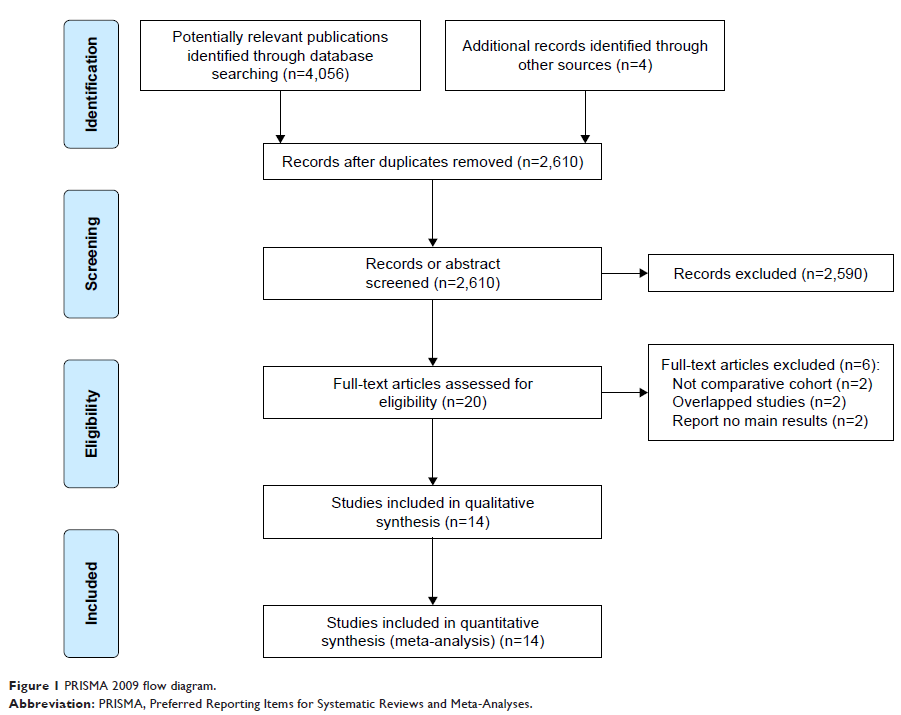
Patients and methods: This review was registered at the International
Prospective Register of Systematic Reviews (number CRD42017075989). Studies in
PubMed, Embase, Web of Science, the Cochrane Library, and ClinicalTrials.gov were thoroughly investigated. Eligible studies included prospective and
retrospective studies evaluating short-term outcomes of minimally invasive
McKeown esophagectomy (MIME) vs minimally invasive Ivor Lewis esophagectomy
(MILE) in patients with resectable esophageal or junctional tumors. Main
parameters included anastomotic leak and 30-day/in-hospital mortality. Overall
incidence rates (ORs)/weighted mean difference (WMD) with 95% confidence
intervals (CIs) were calculated by employing random-effects models.
Results: Fourteen studies containing 3,468 cases were
included in this meta-analysis. Age, male sex, and American Joint Committee on
Cancer (AJCC) stage between the 2 groups were not statistically different. MIME
led to more blood loss, longer operating time, and longer hospital stay than
MILE. MIME was associated with higher incidence of pulmonary complications (OR
=1.96, 95% CI =1.28–3.00) as well as total anastomotic leak (OR =2.55, 95% CI
=1.40–4.63), stricture (OR =2.07, 95% CI =1.05–4.07), and vocal cord
injury/palsy (OR =5.62, 95% CI =3.46–9.14). In addition, the differences of R0
resection rate, number of lymph modes retrieved, blood transfusion rate, length
of intensive care unit stay, incidence of cardiac arrhythmia, and Chyle leak
between MIME and MILE were not statistically significant. Notably, incidence of
severe anastomotic leak (OR =1.28, 95% CI =0.73–2.24) and 30-day/in-hospital
mortality (OR =1.76, 95% CI =0.92–3.36) as well as 90-day mortality (OR =2.22,
95% CI =0.71–6.98) between the 2 procedures were also not significantly
different.
Conclusion: This study suggests that MIME and MILE are
comparable with respect to clinical safety. MILE may be a better option when
oncologically and clinically suitable. MIME is still a safe alternative
procedure when clinically indicated. However, this evidence is at risk for
bias; randomized controlled trials are needed to validate or correct our
results.
Keywords: Ivor Lewis
esophagectomy, McKeown esophagectomy, minimally invasive esophagectomy (MIE),
cervical anastomosis, intrathoracic anastomosis