9 1 2 3 6
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

2010-2017 年中国上海一家三级医院对碳青霉烯耐药革兰氏阴性杆菌引起的血流感染的各种抗微生物治疗方案的现实世界研究
Authors Tan J, Yu W, Wu G, Shen J, Fang Y, Zhu H, Xiao Q, Peng W, Lan Y, Gong Y
Received 27 January 2020
Accepted for publication 16 June 2020
Published 21 July 2020 Volume 2020:13 Pages 2453—2463
DOI https://doi.org/10.2147/IDR.S247378
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Background: We conducted a real-world analysis of the effectiveness of different antibiotic regimens for bloodstream infections (BSIs) caused by carbapenem-resistant gram-negative bacilli (CR-GNB) in a Chinese population.
Methods: A retrospective observational study was conducted between January 2010 and December 2017. Patients with BSIs caused by CR-GNB confirmed by in vitro susceptibility tests were enrolled, and patient medical record data on antimicrobial agents and microbiological and clinical outcomes were extracted.
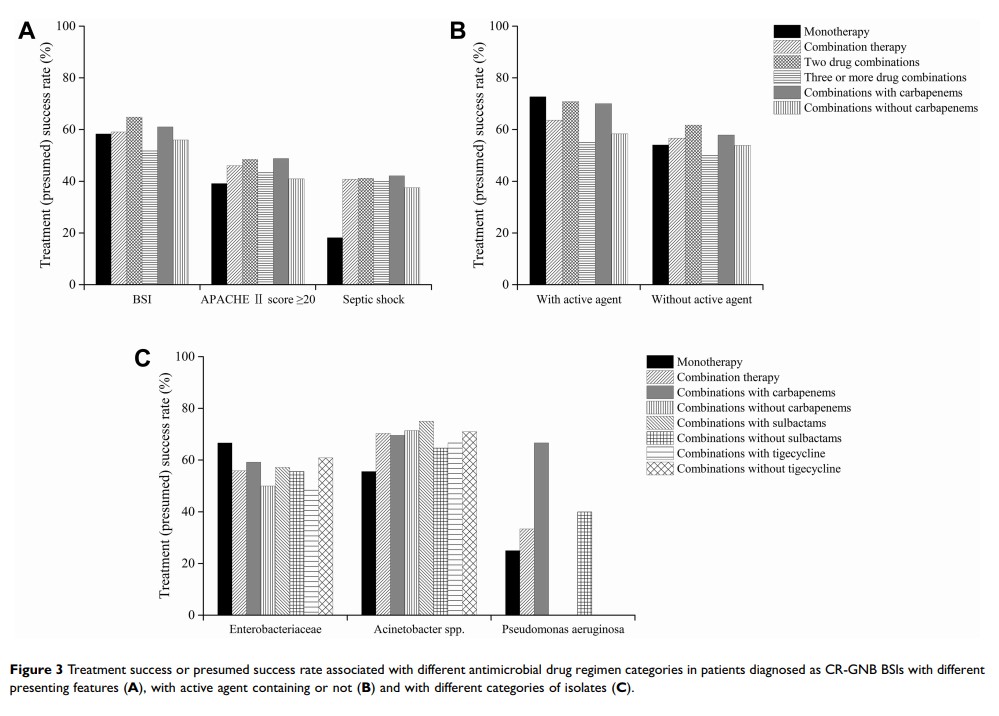
Results: A total of 175 individuals were included; 127 individuals (72.6%) received combination therapy (two or more antibiotics), while 48 individuals (27.4%) received monotherapy (single antibiotic). The all-cause 28-day mortality was 20.0%. Treatment success or presumed success rates were very similar between the monotherapy and combination therapy groups (58.3% versus 59.1%; P = 0.931). Combination therapy had a higher success rate trend than monotherapy in septic shock patients (40.7% versus 18.2%; P = 0.268). Improved therapeutic effects were observed in the active agent-containing group, although the differences were not significant.
Conclusion: Combination therapy likely has better therapeutic effects on critical BSIs caused by CR-GNB than monotherapy. Choosing a proper active agent in an antimicrobial regime is relatively crucial to the ultimate treatment outcome.
Keywords: bloodstream infection, carbapenem-resistant gram-negative bacilli, antimicrobial regimen, treatment success rate, real-world, Chinese population