9 1 2 3 6
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

已发表论文
与再生障碍性贫血有关的血清阴性乙肝治疗的免疫抑制治疗疗效与安全性
Authors Chen HF, Xu BX, Shen HS, Li ZY, Jin LJ, Tang JQ, Wang J, Zhu JJ, Qin LM, Cui QY, Ren YY, Wu TQ
Published Date September 2014 Volume 2014:8 Pages 1299—1305
DOI http://dx.doi.org/10.2147/DDDT.S67908
Received 18 May 2014, Accepted 3 July 2014, Published 9 September 2014
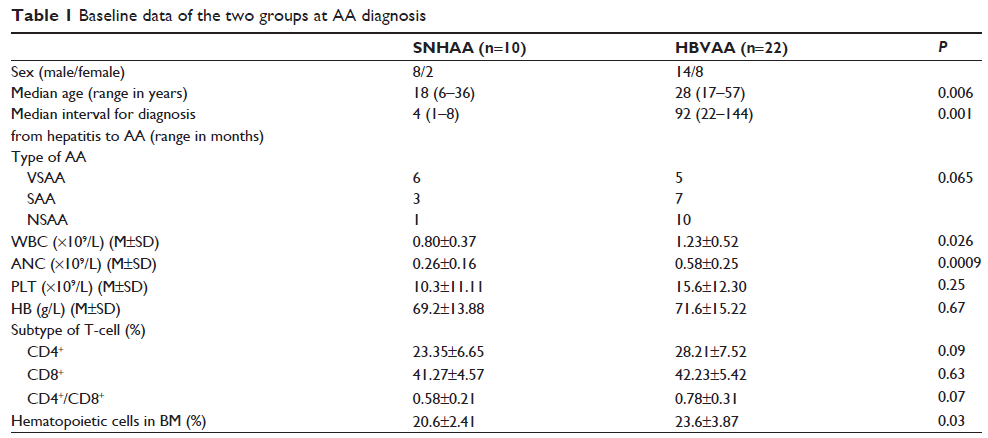
Objective: To investigate the clinical characteristics of seronegative hepatitis-associated aplastic anemia (AA) (SNHAA) and hepatitis B virus (HBV) infection complicating AA (HBVAA), and thereby compare the efficacy of immunosuppressive therapy (IST).
Methods: An analysis was conducted on the clinical data of ten patients with SNHAA out of 332 cases of AA from our center at AA diagnosis, and on the efficacy of IST. This was compared to 22 cases of HBVAA at AA onset as well as the associated IST outcomes.
Results: Nine patients with SNHAA developed severe aplastic anemia, with a median age of 18 years. After IST, six (60%) of the SNHAA patients achieved complete remission and two achieved partial remission. The patients with HBVAA had a total response rate of 82.3%. The disease recurred in two HBVAA patients. No statistically significant differences were observed in response rate, mortality, and recurrence rate between both groups. As compared with HBVAA, patients with SNHAA had a shorter interval from the acute episode of hepatitis to AA onset (4 months versus 92 months, P =0.00), a quicker response to IST (2.5 months versus 4.5 months, P =0.018), a lower proportion of bone marrow hematopoietic tissues (20.6% versus 23.6%, P =0.03), and lower white blood cell and absolute neutrophil count (0.8×109/L versus 1.23×109/L and 0.26×109/L versus 0.58×109/L, P =0.026 and P =0.0009, respectively). No significant liver damage or hepatitis B fulminant infection was observed in either group during the follow-up.
Conclusion: The prevalence of SNHAA is 3.01%. SNHAA often presents as severe AA and responds to IST quickly. Neither hepatitis prior to AA nor AA complicating HBV infection have been shown to influence the early efficacy of IST and adverse events, and HBV may not be the causative agent of AA.
Keywords: hepatitis-associated aplastic anemia, hepatitis B infection, liver injury
Methods: An analysis was conducted on the clinical data of ten patients with SNHAA out of 332 cases of AA from our center at AA diagnosis, and on the efficacy of IST. This was compared to 22 cases of HBVAA at AA onset as well as the associated IST outcomes.
Results: Nine patients with SNHAA developed severe aplastic anemia, with a median age of 18 years. After IST, six (60%) of the SNHAA patients achieved complete remission and two achieved partial remission. The patients with HBVAA had a total response rate of 82.3%. The disease recurred in two HBVAA patients. No statistically significant differences were observed in response rate, mortality, and recurrence rate between both groups. As compared with HBVAA, patients with SNHAA had a shorter interval from the acute episode of hepatitis to AA onset (4 months versus 92 months, P =0.00), a quicker response to IST (2.5 months versus 4.5 months, P =0.018), a lower proportion of bone marrow hematopoietic tissues (20.6% versus 23.6%, P =0.03), and lower white blood cell and absolute neutrophil count (0.8×109/L versus 1.23×109/L and 0.26×109/L versus 0.58×109/L, P =0.026 and P =0.0009, respectively). No significant liver damage or hepatitis B fulminant infection was observed in either group during the follow-up.
Conclusion: The prevalence of SNHAA is 3.01%. SNHAA often presents as severe AA and responds to IST quickly. Neither hepatitis prior to AA nor AA complicating HBV infection have been shown to influence the early efficacy of IST and adverse events, and HBV may not be the causative agent of AA.
Keywords: hepatitis-associated aplastic anemia, hepatitis B infection, liver injury