9 0 8 0 2
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 2.6 Breast Cancer (Dove Med Press)
- 3.9 Clin Epidemiol
- 3.3 Cancer Manag Res
- 3.9 Infect Drug Resist
- 3.6 Clin Interv Aging
- 4.8 Drug Des Dev Ther
- 2.8 Int J Chronic Obstr
- 8.0 Int J Nanomed
- 2.3 Int J Women's Health
- 3.2 Neuropsych Dis Treat
- 4.0 OncoTargets Ther
- 2.2 Patient Prefer Adher
- 2.8 Ther Clin Risk Manag
- 2.7 J Pain Res
- 3.3 Diabet Metab Synd Ob
- 4.3 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.9 Pharmgenomics Pers Med
- 3.5 Risk Manag Healthc Policy
- 4.5 J Inflamm Res
- 2.3 Int J Gen Med
- 4.1 J Hepatocell Carcinoma
- 3.2 J Asthma Allergy
- 2.3 Clin Cosmet Investig Dermatol
- 3.3 J Multidiscip Healthc

癌胚抗原预测接受预防性颅脑照射治疗的小细胞肺癌患者脑转移发生率和生存率的临床价值
Authors Guo D, Jing W, Zhu H, Li MH, Zou B, Zhang Y, Fu L, Kong L, Yue J, Yu J
Received 23 May 2018
Accepted for publication 1 August 2018
Published 4 September 2018 Volume 2018:10 Pages 3199—3205
DOI https://doi.org/10.2147/CMAR.S175043
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
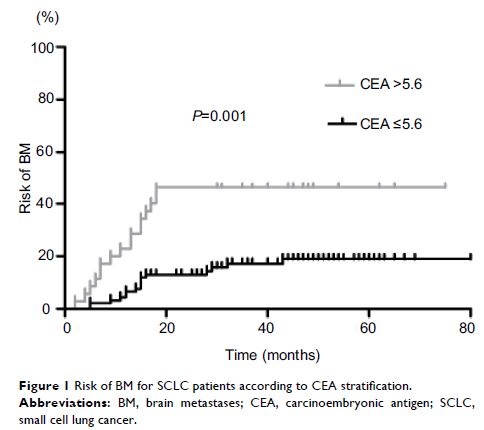
Background: Although the role of prophylactic cranial irradiation (PCI) in the treatment of small cell lung cancer (SCLC) has been confirmed, the occurrence of brain metastases (BM) in patients remains a major problem. We designed this study to evaluate the clinical value of carcinoembryonic antigen (CEA) for predicting the incidence of BM and survival in SCLC patients who received PCI.
Materials and methods: The records of 128 consecutive SCLC patients, who underwent PCI in our institute between 2005 and 2015, were analyzed. The collected data included clinicopathological features and the levels of CEA, neuron-specific enolase (NSE), cytokeratin 19 fragments (CYFRA21-1), and albumin. Kaplan–Meier and Cox regression analyses were used to determine the factors that affect BM and survival in SCLC patients after PCI.
Results: In total, 128 patients were identified, with a median (range) age of 62 (30–83) years. Thirty-two patients developed BM at some time during follow-up. The median levels of CEA, NSE, CYFRA21-1, and albumin were 7.6 ng/mL, 44 ng/mL, 4.6 ng/mL, and 42.1 g/L, respectively. In the multivariate analysis, CEA level (HR: 2.479, 95% CI: 1.101–5.581; P =0.028), advanced clinical stage (HR: 2.929, 95% CI: 1.338–6.413; P =0.007), and NSE level (HR: 3.021, 95% CI: 1.226–7.442; P =0.016) were significantly correlated with BM. CEA (HR: 1.903, 95% CI: 1.133–3.195; P =0.015) and advanced clinical stage (HR: 2.002, 95% CI: 1.227–3.267; P =0.005) were independently associated with worse overall survival in SCLC patients.
Conclusion: CEA is an independent predictive factor for the incidence of BM after PCI in SCLC and can be used as a predictor of BM in SCLC. In addition, a high level of CEA indicates a poor prognosis in SCLC patients after PCI. Prospective randomized clinical studies are required to confirm these findings.
Keywords: carcinoembryonic antigen, brain metastases, predicting, survival, small cell lung cancer