111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

2002-2017 年间从中国患者分离的碳青霉烯耐药的大肠杆菌的分子机制和流行病学
Authors Tian X, Zheng X, Sun Y, Fang R, Zhang S, Zhang X, Lin J, Cao J, Zhou T
Received 21 September 2019
Accepted for publication 30 January 2020
Published 17 February 2020 Volume 2020:13 Pages 501—512
DOI https://doi.org/10.2147/IDR.S232010
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Background: The emergence and spread of carbapenem-resistant Escherichia coli (E. coli ) pose a serious threat to human health worldwide. This study aimed to investigate the molecular mechanisms underlying carbapenem resistance and their prevalence among E. coli in China.
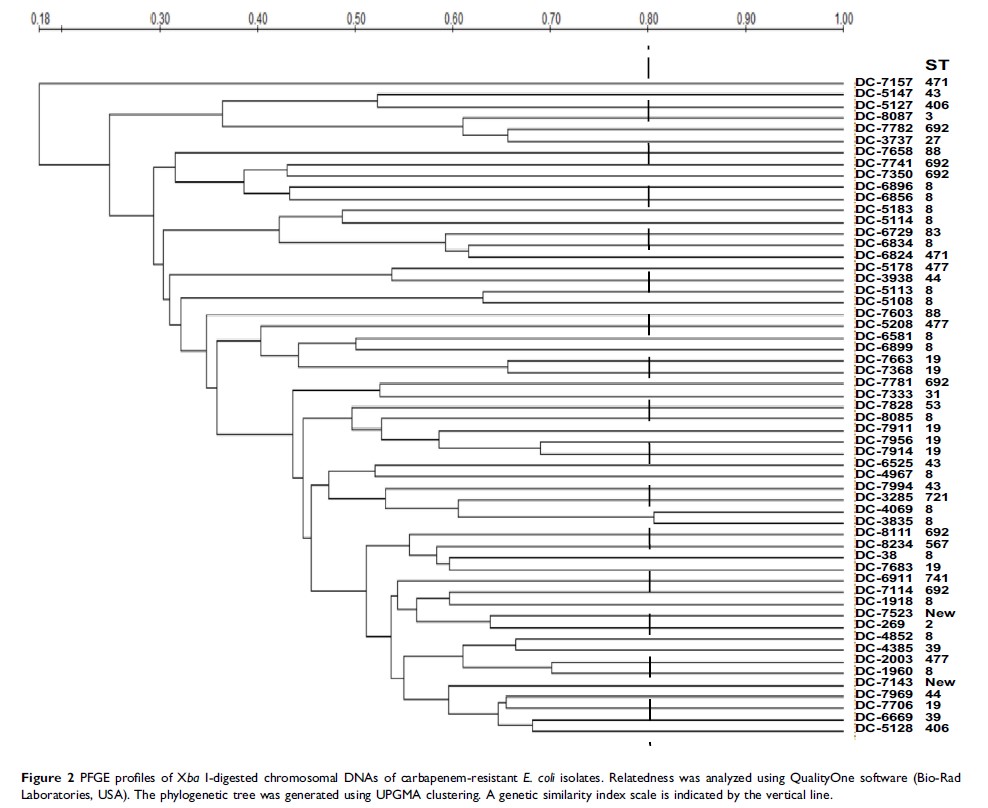
Methods: A collection of 5796 E. coli clinical isolates were collected from the First Affiliated Hospital of Wenzhou Medical University from 2002 to 2017. Sensitivity to antibiotics was determined using the agar dilution method. The detection of carbapenemases production and the prevalence of resistance-associated genes were investigated through modified carbapenem inactivation method (mCIM), PCR and sequencing. The mutations in outer membrane porins genes (ompC and ompF ) were also analyzed by PCR and sequencing assays. The effect of efflux pump mechanism on carbapenem resistance was also tested. E. coli were typed by pulsed-field gel electrophoresis (PFGE) and multilocus sequence typing (MLST).
Results: A total of 58 strains (1.0%) of carbapenem-resistant E. coli were identified. The strains carrying bla KPC-2 and bla NDM accounted for 22.4% (13/58) and 51.7% (30/58), respectively. Among bla NDM- positive strains, 27 bla NDM genes were assigned to bla NDM-5, while the remaining three strains were bla NDM-1, whereas bla VIM, bla IMP, bla OXA-48, and bla SHV were not found. The CTX-M-type β-lactamase genes accounted for 96.6% (56/58). In addition, bla TEM-1 genes were identified in 58.6% of tested strains. In carbapenem-resistant isolates, mutations in OmpC (the majority of mutated sites were D192G and Q104_F141del, accounting for 54.5%) and OmpF (large deletions S75_V127del, W83_D135del and Q88_D135del) were detected. Of note, the antibiotic resistance was not associated with overexpression of efflux pump. Moreover, MLST categorized the 58 carbapenem-resistant isolates into 19 different sequence types. PFGE analysis revealed that homology among the carbapenem-resistant isolates was low and sporadic.
Conclusion: The bla NDM was the principal resistance mechanism of carbapenem-resistant E. coli in the hospital. bla NDM-5 is becoming a new threat to public health and the alteration of outer membrane porins might help further increase the MIC of carbapenem.
Keywords: Escherichia coli , carbapenem-resistant, carbapenemase, outer membrane porin, epidemiology