111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

经皮冠状动脉介入治疗的慢性完全闭塞病变患者冠状动脉慢血流和无复流现象的发生率、预测因素和预后
Authors Wang Y, Zhao H, Wang C, Zhang X, Tao J, Cui C, Meng Q, Zhu Y, Luo D, Hou A, Luan B
Received 5 October 2019
Accepted for publication 4 February 2020
Published 18 February 2020 Volume 2020:16 Pages 95—101
DOI https://doi.org/10.2147/TCRM.S233512
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Background: The incidence and prognosis of coronary slow-flow (CSF) and no-reflow phenomenon (NRP) in patients with coronary chronic total occlusion (CTO) who underwent percutaneous coronary intervention (PCI) remain unclear.
Methods: This single-center prospective study aimed to investigate the incidence of CSF/NRP during CTO interventional therapy, determine predictors of CSF/NRP, and evaluate its effect on patient outcomes.
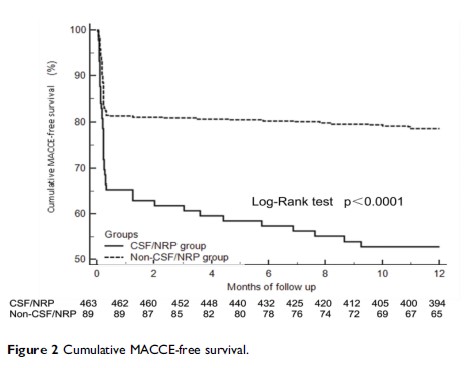
Results: In this study, 552 patients with CTO who underwent PCI were included. CSF/NRP occurred in 16.1% of them. They had higher incidences of diabetes mellitus (53.9% vs 36.3%, p =0.002) and hypertension (50.6% vs 37.1%, p =0.018) and a lower incidence of retrograde filling grade > 2 (34.8% vs 47.1%, p =0.036). Patients with CSF/NRP had a higher neutrophil ratio (55.6± 19.4 vs 52.4± 18.3, p =0.038) and levels of low-density lipoprotein (LDL; 3.0± 0.8 vs 2.8± 0.6, p =0.029), fasting glucose (FG; 8.3± 1.3 vs 6.8± 1.1, p =0.005), uric acid (332.6± 82.9 vs 308.2± 62.8, p =0.045), and high-sensitivity C-reactive protein (Hs-CRP; 9.8± 4.8 vs 7.3± 3.9, p =0.036). A multivariate logistic regression analysis revealed that diabetes mellitus (odds ratio [OR], 1.962; 95% confidence interval [CI]: 1.198– 2.721; p =0.042), mean platelet volume (MPV; OR,1.284; 95% CI, 1.108– 1.895; p =0.046), LDL cholesterol (LDL-C; OR, 1.383; 95% CI, 1.105– 2.491; p =0.036), FG (OR, 2.095; 95% CI, 1.495– 2.899; p =0.018), Hs-CRP (OR, 2.218; 95% CI, 1.556– 3.519; p =0.029), and retrograde filling of grade > 2 (OR, 0.822; 95% CI, 0.622– 0.907; p =0.037) were independent predictors of CSF/NRP in CTO patients who underwent PCI. Kaplan-Meier analysis revealed that the patients in the CSF/NRP group had a significantly lower cumulative major cardiac and cerebrovascular events (MACCE)-free survival than those in the non-CSF/NRP group (p < 0.0001).
Conclusion: Of the patients with CTO who underwent PCI, 16.1% developed CSF/NRP and had a significantly lower cumulative MACCE-free survival rate. Diabetes mellitus; higher levels of MPV, LDL-C, FG, and Hs-CRP; and a lower incidence of retrograde filling grade > 2 were independent predictors of CSF/NRP in CTO patients who underwent PCI. Thus, they can be used for risk stratification.
Keywords: coronary slow-flow, no-reflow phenomenon, coronary chronic total occlusion, PCI, prognosis