111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

治疗前全身炎症反应指数作为新辅助化学疗法治疗的乳腺癌患者有用的预后指标
Authors Chen L, Kong X, Wang Z, Wang X, Fang Y, Wang J
Received 21 October 2019
Accepted for publication 14 February 2020
Published 3 March 2020 Volume 2020:12 Pages 1543—1567
DOI https://doi.org/10.2147/CMAR.S235519
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
Background and Objective: Systemic inflammation response index (SIRI=N×M/L), based on neutrophil (N), monocyte (M), and lymphocyte (L) counts, is used to predict the survival of patients with malignant tumors and can fully evaluate the balance between host immune and inflammatory condition. The present study is aimed to evaluate the potential prognostic significance of SIRI in patients with breast cancer undergoing neoadjuvant chemotherapy.
Subjects and Methods: A total of 262 breast cancer patients treated with neoadjuvant chemotherapy were enrolled in this retrospective study. The optimal cutoff value of SIRI by receiver operating characteristic curve stratified patients into low SIRI (< 0.85× 109/L) group and high SIRI (≥ 0.85× 109/L) group. The associations between breast cancer and clinicopathological variables by SIRI were determined by chi-square test or Fisher’s exact test. Kaplan–Meier plots and log-rank test were used to evaluate the clinical outcomes of disease-free survival (DFS) and overall survival (OS). Univariate and multivariate Cox proportional hazards regression models were used to analyze the prognostic value of SIRI. The toxicity of neoadjuvant chemotherapy was evaluated by the National Cancer Institute Common Toxicity Criteria (NCICTC).
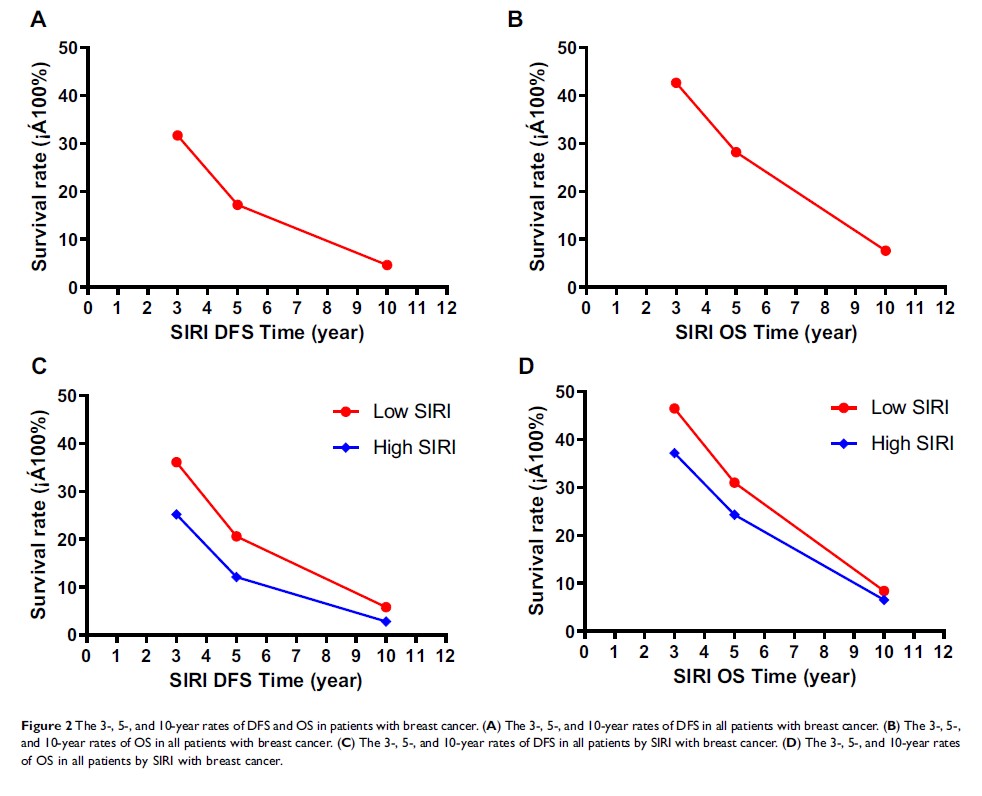
Results: The results were shown that SIRI had prognostic significance by optimal cutoff value of 0.85× 109/L on DFS and OS in univariate and multivariate Cox regression survival analyses. Compared with patients who had high SIRI, patients with low SIRI had longer DFS and OS (41.27 vs 30.45 months, HR: 1.694, 95% CI: 1.128– 2.543, P=0.011; 52.86 vs 45.75 months, HR: 1.288, 95% CI: 0.781– 3.124, P=0.002, respectively). The patients with low SIRI had better 3-, 5-, and 10-year rates of DFS and OS than those with high SIRI. The common toxicities after neoadjuvant chemotherapy were hematologic and gastrointestinal reaction, and the SIRI had no significance on toxicities of all enrolled patients, excepted diarrhea. In patients without neural invasion, those with low SIRI had better prognosis and lower recurrence rates than those with high SIRI.
Conclusion: Pretreatment SIRI with the advantage of repeatable, convenient, and non-invasive is a useful prognostic indicator for breast cancer patients who received neoadjuvant chemotherapy and is a promising biomarker for breast cancer on treatment strategy decisions.
Keywords: systemic inflammation response index, SIRI, breast cancer, neoadjuvant chemotherapy, survival, prognosis