111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

脑卒中后抑郁症大鼠 BDNF-HA2TAT/AAV 经鼻给药的抗抑郁作用及机制的研究
Authors Chen C, Dong Y, Liu F, Gao C, Ji C, Dang Y, Ma X, Liu Y
Received 16 August 2019
Accepted for publication 21 January 2020
Published 4 March 2020 Volume 2020:16 Pages 637—649
DOI https://doi.org/10.2147/NDT.S227598
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Yu-Ping Ning
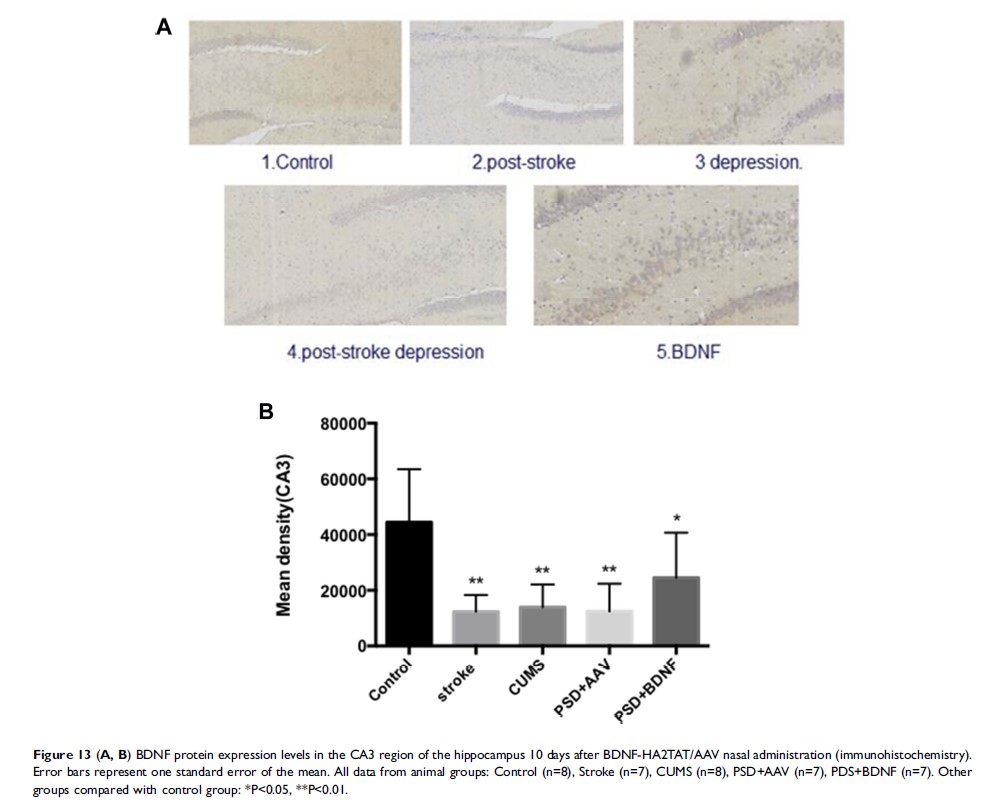
Aim: Post-stroke depression (PSD) is one of the most frequent neuropsychiatric disorders associated with stroke characterized by depression. The neuroplasticity hypothesis postulates that loss of brain-derived neurotrophic factor (BDNF) plays a major role in pathophysiology of PSD, and restoration of it may represent a critical mechanism underlying antidepressant efficacy.
Methods: In previous studies, we designed a new fusion gene, HA2TAT-BDNF, and cloned it into adenovirus associated virus (AAV) to construct the BDNF-HA2TAT/AAV for the delivery of BDNF to central nervous system (CNS) via nose-brain pathway. In this study, we used it to explore the antidepressant effects on PSD rats through behavioral and various histological methods, and try to find out its specific mechanism.
Results: Compared with the control group, the PSD+AAV group showed decreased sucrose consumption percentage in the sucrose preference test (SPT) (P < 0.001) and prolonged immobility in the forced swimming test (FST) (P=0.000). However, the nasal administration of BDNF-HA2TAT/AAV reversed results of these two behavioral tests (P> 0.05, P > 0.05), showing an adequate antidepressant effect. Compared with the control group, the concentrations of BDNF mRNA and protein in the hippocampus (P< 0.05, P < 0.01) and prefrontal cortex (P < 0.01, P < 0.01) of PSD rats both decreased. Increased BDNF mRNA and protein expression was observed in the prefrontal cortex (P > 0.05, P < 0.05), without notable change in the hippocampus (P < 0.05, P < 0.001) of PSD+BDNF rats.
Conclusion: These results suggest that BDNF reductions in the prefrontal cortex and hippocampus are associated with the development of post-stroke depression, and that increased levels of BDNF in the prefrontal cortex could be used as a therapeutic target to treat PSD. However, the exact mechanism of BDNF action remains unclear in this regard, hindering the wider application of our method. We expect that our research could facilitate the exploration of pathogenesis and the new treatment method of PSD.
Keywords: post-stroke depression, PSD, BDNF-HA2TAT/AAV, nasal-brain pathway, hippocampus, prefrontal cortex