111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国一家教学医院中接受多种广谱抗生素治疗的住院患者的前体药耐药的肺炎克雷伯菌 ST11 型分离株的迅速出现
Authors Xu J, Zhao Z, Ge Y, He F
Received 22 December 2019
Accepted for publication 2 March 2020
Published 10 March 2020 Volume 2020:13 Pages 799—804
DOI https://doi.org/10.2147/IDR.S243334
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Eric Nulens
Purpose: Pandrug-resistant K. pneumoniae is still rare in China, and the lack of studies limits our understanding of the emergence mechanism of pandrug-resistant K. pneumoniae . Here, we report the rapid emergence of a pandrug-resistant K. pneumoniae ST11 strain in an inpatient after treatment with multiple broad-spectrum antibiotics in China.
Patients and Methods: K. pneumoniae strain KP65 was isolated from a 55-year-old male patient hospitalized in the Department of Intensive Care Unit (ICU) of a teaching hospital in China. Antimicrobial susceptibility testing was conducted according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI). The complete genome sequence of the strain was determined using the Illumina NovaSeq 6000 platform and long-read MinION sequencer. Genomic features and resistance mechanisms of the strain were comprehensively analysed using various bioinformatics approaches.
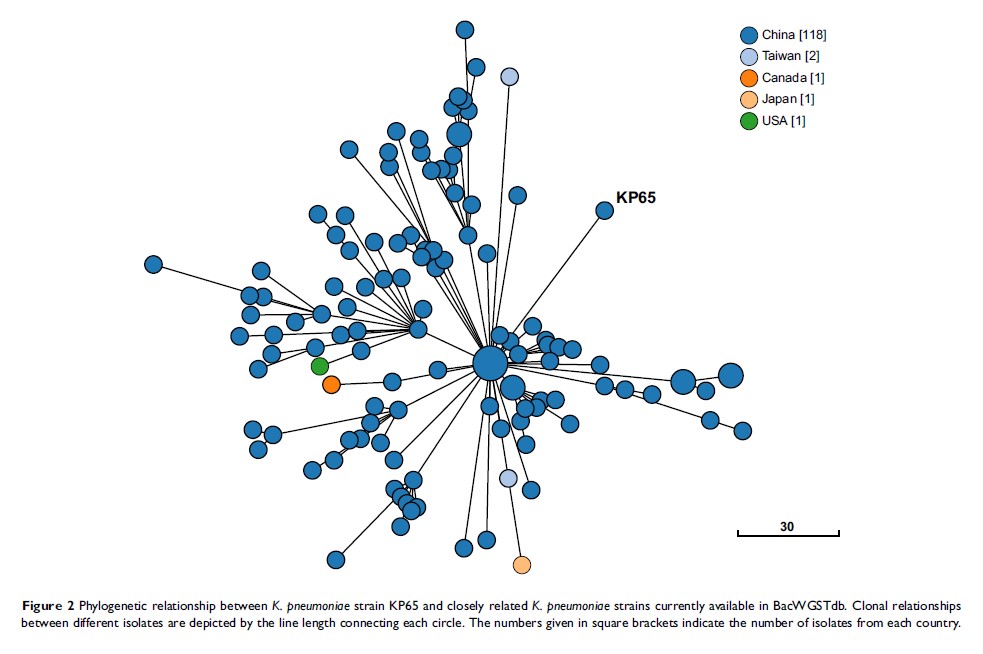
Results: K. pneumoniae strain KP65 was found to be resistant to all antibiotics tested, including beta-lactams, aminoglycosides, quinolones, tigecycline and colistin. Seven resistance genes were identified in the genome. The carbapenem-resistant gene bla KPC-2 and extended-spectrum β-lactamase (ESBL)-producing gene bla CTX-M-65 are located on the IncFII-type plasmid pKPC-2-KP65. No mcr genes were detected in the genome, but an IS 5 insertion element was found at position 117 of the mgrB gene. Regarding the rpsJ gene, single-base substitution, G169C, leading to the amino acid substitution V57L was also identified. According to in silico MLST analysis, K. pneumoniae KP65 belongs to sequence type ST11. The closest relative of K. pneumoniae KP65 is another ST11 K. pneumoniae strain, which was isolated from a bloodstream infection in Hangzhou, differing by only 53 cgMLST loci.
Conclusion: Under the selective pressure of antibiotics, the KPC-2-producing K. pneumoniae ST11 strain can easily evolve pandrug resistance through chromosomal mutations. More attention is required to monitor the prevalence of the KPC-2-producing K. pneumoniae ST11 strain in China.
Keywords: Klebsiella pneumoniae , mgrB , rpsJ , ST11, bla KPC-2