108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

建立简单的列线图以预测早期乳腺癌的腋窝淋巴结转移
Authors Zong Q, Deng J, Ge W, Chen J, Xu D
Received 9 December 2019
Accepted for publication 26 February 2020
Published 18 March 2020 Volume 2020:12 Pages 2025—2035
DOI https://doi.org/10.2147/CMAR.S241641
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Chien-Feng Li
Purpose: Axillary lymph node (ALN) involvement is an important prognostic factor of early invasive breast cancer. The objective of this study was to establish simple nomograms for predicting ALN involvement based on ultrasound (US) characteristics and evaluate the predictive value of US in the detection of ALN involvement.
Patients and Methods: A total of 1328 patients with cT1-2N0 breast cancer by physical exam were retrospectively analyzed. Univariate analysis was used for the comparison of variables, and multivariate analysis was performed by binary logistic regression analysis. The R software was used to establish simple nomograms based on the US characteristics alone. The receiver operating characteristic (ROC) curves of the prediction model and the verification group were drawn, and the area under the curve (AUC) was calculated to evaluate the discrimination of the prediction model. A calibration curve was plotted to assess the nomogram predictions vs the actual observations of the ALN metastasis rate and axillary tumor burden rate.
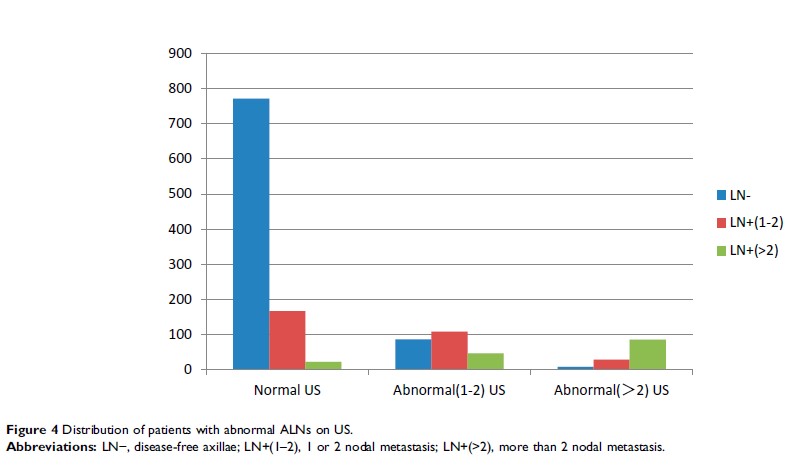
Results: The ALN metastasis rates of the training group and the validation group were 35.1% and 34.1%, respectively. Multivariate analysis showed that molecular subtype, lymphovascular invasion, mass descriptors (size, margin, microcalcification and blood flow signal) and LN descriptors (shape, cortical thickness and long-to-short ratio) were independent impact factors in early breast cancer. The AUC of ALN metastasis rate of prediction model based on US features was 0.802, the AUC of high tumor burden rate was 0.873, and the AUC of external validation group was 0.731 and 0.802, respectively. The calibration curve of the nomogram showed that the nomogram predictions are consistent with the actual metastasis rate and the high tumor burden rate. The results showed that preoperative US had a sensitivity of 59.4% and a specificity of 88.9% for predicting the ALN metastasis rate.
Conclusion: The successfully established nomograms based on US characteristics to predict ALN metastasis rate and high axillary tumor burden rate in early breast cancer can achieve individual prediction. Compared with other nomogram predictions, it is more intuitive, and can help clinical decision-making; thus, it should be promoted. However, at this time US features alone are insufficient to replace sentinel lymph node biopsy.
Keywords: axillary lymph node involvement, early breast cancer, ultrasound, nomogram