108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

治疗前白蛋白与碱性磷酸酶比例在广泛期小细胞肺癌中的预后价值:一项回顾性队列研究
Authors Zhou S, Wang H, Jiang W, Yu Q, Zeng A
Received 1 February 2020
Accepted for publication 11 March 2020
Published 18 March 2020 Volume 2020:12 Pages 2015—2024
DOI https://doi.org/10.2147/CMAR.S247967
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Eileen O'Reilly
Purpose: Evidence regarding the relationship between albumin-to-alkaline phosphatase ratio (AAPR) and overall survival (OS) in extensive-disease small-cell lung cancer (ED-SCLC) patients is limited. This study aimed to investigate whether AAPR was independently related to OS in ED-SCLC patients after adjusting for potential covariates.
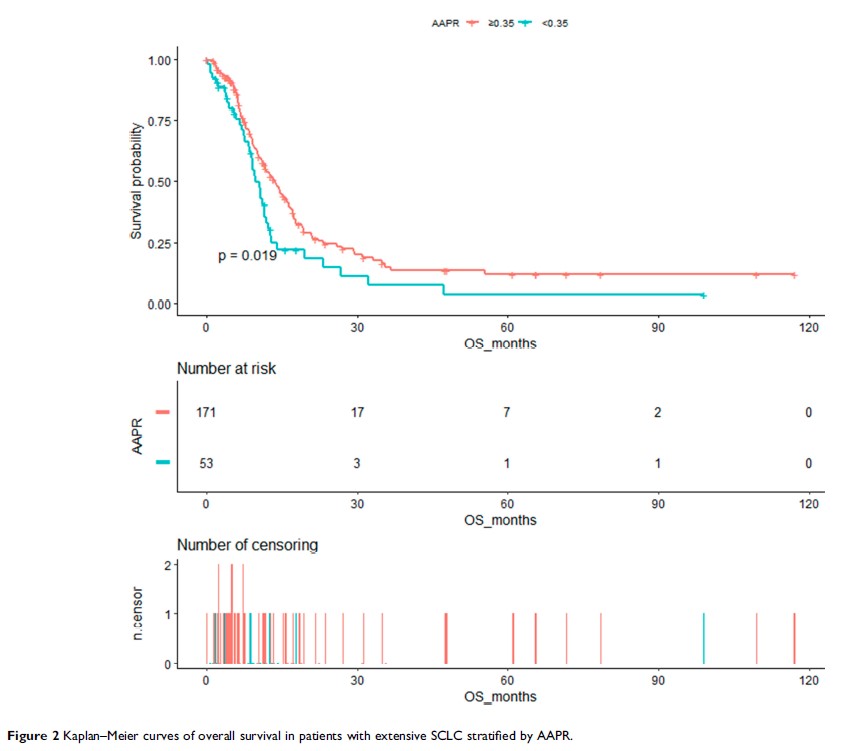
Patients and Methods: This was a retrospective cohort study of 224 patients with ED-SCLC. The target independent and dependent variables were pretreatment AAPR and OS, respectively. Covariates included age; sex; Eastern Cooperative Oncology performance status score; smoking history; existence of metastasis to organs such as the bone, lung, liver, brain, malignant plural effusion and others; sum of organ metastasis (≤ 3, > 3), evaluation of first-line treatment; and sum of treatment lines (< 2, ≥ 2). Student’s t test or chi-squared test was used to analyze the associations between AAPR and clinical characteristics. Kaplan–Meier survival analysis and Cox’s proportional hazards regression model were used to assess the prognostic value of AAPR for OS.
Results: The average patient age was 60.51± 8.73 years, and 87.95% were men. A non-linear relationship between AAPR and OS was detected, with an inflection point of 0.35. The hazard ratios (HRs) of the left (AAPR < 0.35) and right sides (AAPR ≥ 0.35) of inflection point were 0.04 (95% CI=0.00– 0.70, p =0.0268) and 0.52 (95% CI=0.16– 1.64, p =0.2659), respectively. Kaplan–Meier analysis showed a median OS of 9.73 months (95% CI=8.6– 12.33) for AAPR < 0.35 and 13.7 months (95% CI=11.43– 16.37) for AAPR ≥ 0.35 (log-rank p < 0.0001). The Cox proportional hazards model showed that AAPR < 0.35 increased the risk of death after adjusting for potential confounders (HR=1.65, 95% CI=1.11– 2.46). In subgroup analysis, the trends of HRs were increased across all subgroups with AAPR < 0.35 after stratification.
Conclusion: Pretreatment AAPR might be served as an independent prognostic indicator in ED-SCLC patients. Our findings should be further validated in large-scale and prospective clinical trials.
Keywords: AAPR, overall survival, prognosis, extensive-disease small-cell lung cancer