111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

2003 年至 2016 年中国温州碳青霉烯耐药的肺炎克雷伯菌的动态流行病学和毒力特性
Authors Zhao Y, Zhang S, Fang R, Wu Q, Li J, Zhang Y, Rocker A, Cao J, Lithgow T, Zhou T
Received 19 December 2019
Accepted for publication 3 March 2020
Published 31 March 2020 Volume 2020:13 Pages 931—940
DOI https://doi.org/10.2147/IDR.S243032
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Sahil Khanna
Purpose: To investigate transitions in resistance mechanisms, virulence characteristics and molecular epidemiology of carbapenem-resistant Klebsiella pneumoniae (CRKP) during 2003– 2016 in a major Eastern Chinese medical center.
Patients and Methods: From a total of 2299 K. pneumoniae clinical strains collected from 2003 to 2016, 214 were found to be CRKP isolates and were selected for further study. Characterization of these was conducted by molecular detection of antibiotic resistance markers and virulence determinants, modified carbapenem inactivation method and multilocus sequence typing (MLST).
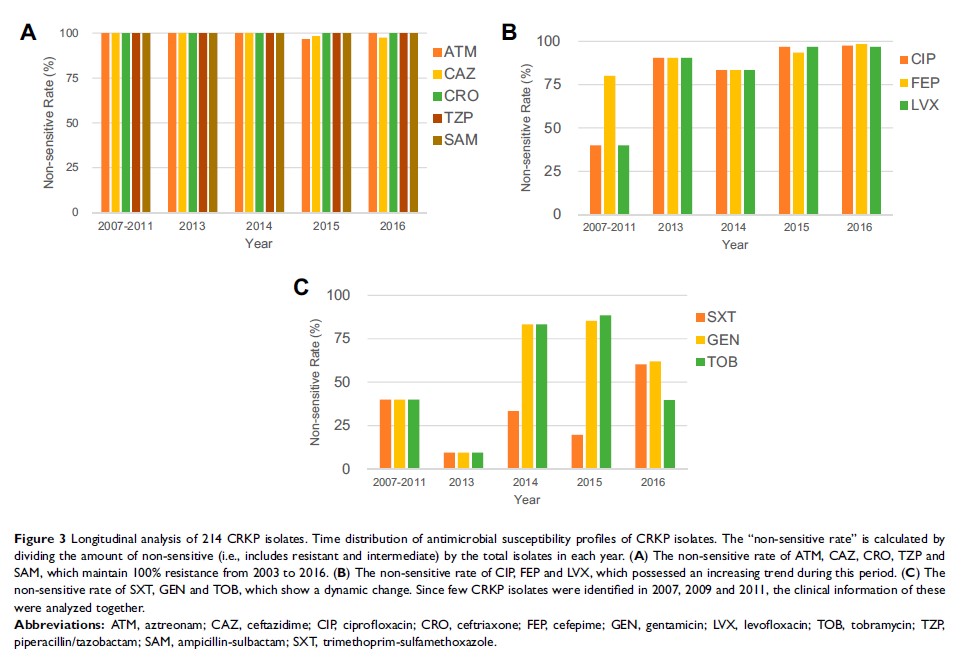
Results: In this study, the prevalence of CRKP was increasing over the 14-year period, mirroring a national trend. These CRKP strains were resistant to most of the tested, clinically relevant drugs. The majority of these CRKP strains were positive for carbapenemases, with the Klebsiella pneumoniae carbapenemase (KPC) found to be the dominant type (207/210, 98.6%). The carrier rates of virulence genes uge, entB, fimH, mrkD and ureA increased in 2016, while the ybtA, iucA and irp2 showed a relatively constant trend. From MLST data, ST11 (88.8%, 190/214) was the preponderant sequence type (ST), followed by ST15 (1.9%, 4/214) and ST656 (1.4%, 3/214). Several strains with less common STs (ST690, ST895, ST1823 and ST1384) were also detected, and these too showed high levels of antimicrobial resistance.
Conclusion: The average national rise in CRKP across China is mirrored in this in-depth analysis of a single hospital, while the prevalence of hypervirulent CRKP (such as ST15) was relatively low as of 2016. Continuous monitoring is necessary to keep track of CRKP and should include the prospect of newly emerging strains with less common STs and the prospect of detecting carbapenem-resistant, carbapenemase-negative Klebsiella pneumoniae .
Keywords: Klebsiella pneumoniae , carbapenem-resistant, antimicrobial resistance, ST11, epidemiology