111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

胫骨恶性肿瘤切除术后,通过 3D 打印多孔假体对 “超临界骨缺损” 的修复重建
Authors Zhao D, Tang F, Min L, Lu M, Wang J, Zhang Y, Zhao K, Zhou Y, Luo Y, Tu C
Received 14 January 2020
Accepted for publication 13 March 2020
Published 8 April 2020 Volume 2020:12 Pages 2503—2512
DOI https://doi.org/10.2147/CMAR.S245949
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Ahmet Emre Eskazan
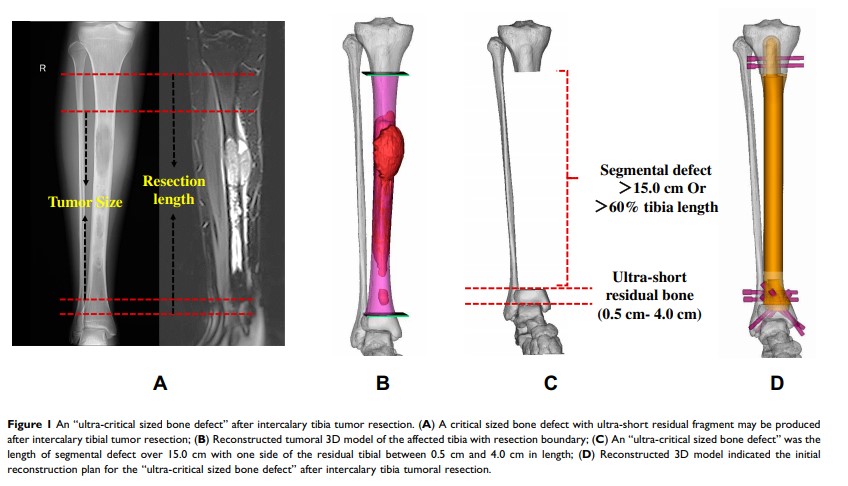
Purpose: This study aimed to evaluate the early stability, limb function, and mechanical complications of 3D-printed porous prosthetic reconstruction for “ultra-critical sized bone defects” following intercalary tibial tumor resections.
Methods: This study defined an “ultra-critical sized bone defect” in the tibia when the length of segmental defect in the tibia was > 15.0 cm or > 60% of the full tibia and the length of the residual fragment in proximal or distal tibia was between 0.5 cm and 4.0 cm. Thus, five patients with “ultra-critical sized bone defects” following an intercalary tibial malignant tumor resection treated with 3D-printed porous prosthesis between June 2014 and June 2018 were retrospectively reviewed. Patient information, implants design and fabrication, surgical procedures, and early clinical outcome data were collected and evaluated.
Results: Among the five patients, three were male and two were female, with an average age of 30.2 years. Pathological diagnoses were two osteosarcomas, one Ewing sarcoma, one pseudo-myogenic hemangioendothelioma, and one undifferentiated pleomorphic sarcoma . The average length of the bone defects following tumor resection was 22.8cm, and the average length of ultra-short residual bone was 2.65cm (range=0.6cm– 3.8cm). The mean follow-up time was 27.6 months (range=14.0– 62.0 months). Early biological fixation was achieved in all five patients. The average time of clinical osseointegration at the bone–porous interface was 3.2 months. All patients were reported to be pain free and have no limitations in their walking distance. No prosthetic mechanical complications were observed.
Conclusion: Reconstruction of the “ultra-critical sized bone defect” after an intercalary tibial tumor resection using 3D-printed porous prosthesis achieved satisfactory overall early biological fixation and limb function. Excellent primary stability and the following rigid biological fixation were key factors for success. The outcomes of this study were supposed to support further clinical application and evaluation of 3D-printed porous prosthetic reconstruction for “ultra-critical sized bone defects” in the tibia.
Keywords: 3D-printed porous, prosthetic reconstruction, intercalary tibial resection, critical sized bone defect