110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

碳青霉烯耐药性肺炎克雷伯菌携带者(通过直肠拭子分析),发生继发性碳青霉烯类耐药肺炎克雷伯菌临床感染的危险因素
Authors Chen X, Liu Q, Liu W, Yan Q
Received 23 January 2020
Accepted for publication 16 April 2020
Published 5 May 2020 Volume 2020:13 Pages 1299—1305
DOI https://doi.org/10.2147/IDR.S247101
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Eric Nulens
Purpose: Carbapenem-resistant Klebsiella pneumoniae (CRKP) infection has become a critical clinical concern for its high mortality. Rectal carriage of CRKP has been reported playing an important role in CRKP infection; however, the extent to which carrier develops clinical CRKP infection is unclear. This study aimed to identify risk factors for developing subsequential CRKP clinical infection in rectal carriers with CRKP.
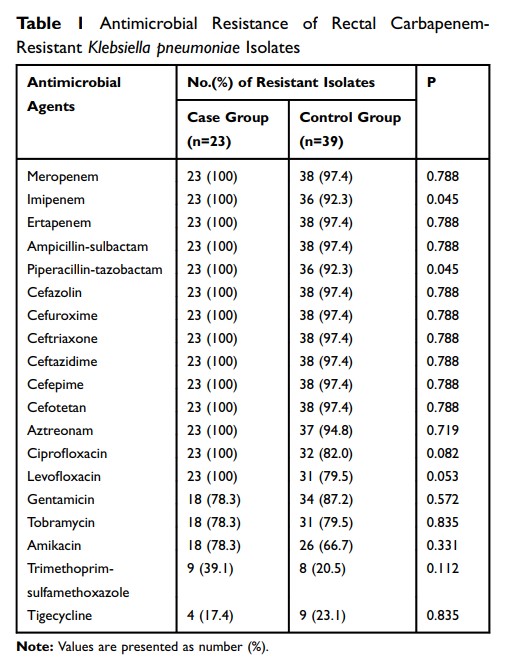
Patients and Methods: Patients were screened for rectal carriage of CRKP in a tertiary university hospital; then, rectal CRKP carriers were divided into case group (those who developed subsequential clinical infection) and control group. Demographics, comorbid conditions, invasive procedures, antimicrobial exposure and other clinical parameters of those two groups were compared and analyzed using univariate and multivariate logistic regression analyses. Antimicrobial susceptibility profile and carbapenemase phenotype/genotype of those CRKP isolates were determined. MLST was applied to elucidate the molecular epidemiology of rectal CRKP isolates and clinical infection ones.
Results: Eight hundred and thirty-five patients were screened for rectal CRKP carriage. A total of 62 CRKP rectal carriers were identified; among them, 37.1% (23/62) developed CRKP clinical infection. CRKP isolates were resistant to most of the tested antimicrobial agents. ST11 was the dominant MLST type in rectal CRKP isolates (71.0%), and all the 23 clinical infection isolates were ST11. Multivariate analysis revealed that admission to the intensive care unit (ICU) (OR, 6.753; P =0.006), being in coma condition (OR, 11.085; P =0.015) and receiving central venous catheter (OR, 8.628; P =0.003) were independent risk factors for progressing to subsequential CRKP infection among those rectal carriers.
Conclusion: This study identified independent risk factors for developing subsequential CRKP clinical infection among CRKP rectal carriers, with being in coma condition as a new finding. It would help clinician target those high-risk rectal CRKP-colonized patients for prevention of subsequential clinical infection.
Keywords: carbapenem-resistant Klebsiella pneumoniae , infection, risk factors, rectal carriage