110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

β 内酰胺/β 内酰胺酶抑制剂(BLBLIs)的复合制剂结合碳青霉烯类对肝硬化合并革兰氏阴性菌血液感染的临床疗效和成本-效果分析
Authors Dong Y, Li Y, Zhang Y, Sun D, Du Q, Zhang T, Teng M, Han R, Wang Y, Zhu L, Lei J, Dong Y, Wang T
Received 9 December 2019
Accepted for publication 4 April 2020
Published 7 May 2020 Volume 2020:13 Pages 1327—1338
DOI https://doi.org/10.2147/IDR.S241648
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Sahil Khanna
Background: Gram-negative bacteria bloodstream infection (GNB-BSI) results in considerable mortality and hospitality costs in cirrhotic patients. β-lactam/β-lactamase inhibitor combinations (BLBLIs) and carbapenems (CARs) are widely recommended for treating GNB-BSI in cirrhotic patients, while the efficacy and cost-effectiveness of two strategies have never been evaluated. Therefore, we conducted a retrospective cohort study to evaluate the efficacy and the cost-effectiveness of BLBLIs and CARs.
Patients and Methods: Cirrhotic patients with GNB-BSI treated by BLBLIs or CARs were included. A propensity score-matching analysis was performed to compare the efficacy between BLBLIs and CARs. A decision tree was used to estimate the clinical outcomes and direct costs of treating BSI using two strategies from the patients’ perspective.
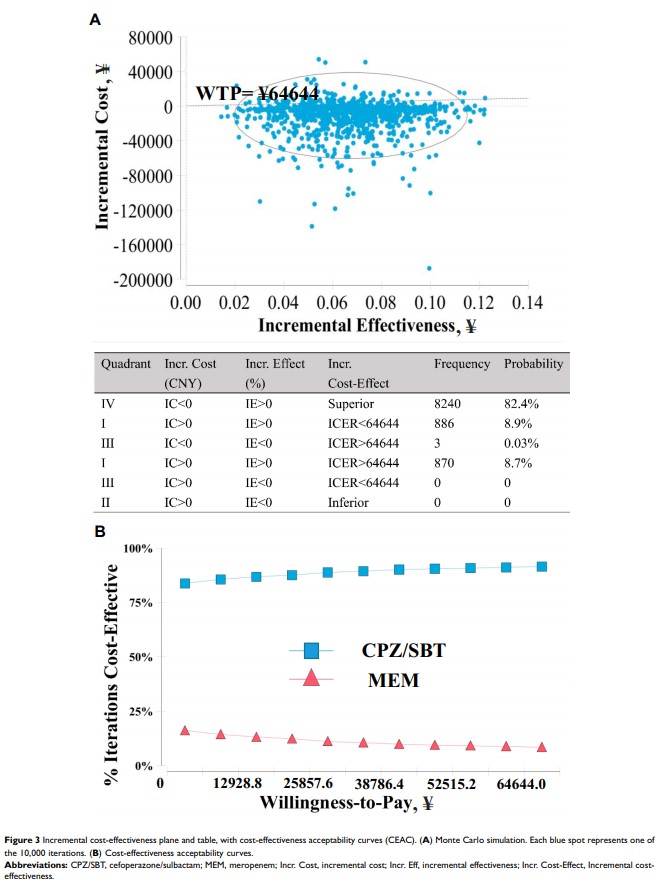
Results: No statistically significant difference was found between the BLBLIs (n = 41) group and the CARs (n = 43) group regarding the time to defervescence (2.4 ± 0.2 vs 2.5 ± 0.3, P = 0.94). Thirty-seven patients from each group were matched in propensity-score-matched cohort, and there was no significant difference between two groups in terms of the time to defervescence (2.4 ± 0.3 vs 2.4 ± 0.3, P = 0.75) and success rate (86.5% vs 78.4%; OR = 0.57; P = 0.36). Based on the drug and hospital costs in China, cefoperazone/sulbactam was cost-effective in the present analysis under the willingness-to-pay threshold (¥ 64,644).
Conclusion: The efficacy of BLBLIs is similar to CARs. Cefoperazone/sulbactam could be a cost-effective therapy in cirrhotic patients with GNB-BSI. Carbapenems-sparing regimens should be encouraged in regions with a low prevalence of MDR bacteria.
Keywords: liver cirrhosis, gram-negative bacteria, bloodstream infection, efficacy, cost-effectiveness