110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

上皮样胶质母细胞瘤的临床病理、免疫组织化学和分子遗传学研究:15 例病例系列及文献综述
Authors Zeng Y, Zhu X, Wang Y, Liu B, Yang X, Wang Q, Du J, Ma Y, Lin L, Fu P, Xiao H, Guo QN
Received 11 February 2020
Accepted for publication 19 April 2020
Published 8 May 2020 Volume 2020:13 Pages 3943—3952
DOI https://doi.org/10.2147/OTT.S249317
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nicola Silvestris
Purpose: To observe the clinicopathological, immunohistochemical, and molecular genetic features of epithelioid glioblastoma (E-GBM), and identify tumor-associated prognostic factors.
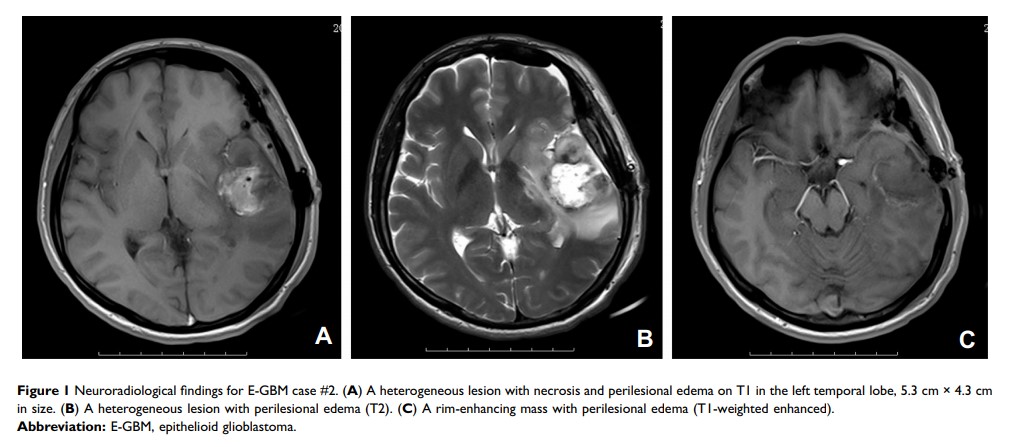
Patients and Methods: The clinical and radiological data of fifteen cases of E-GBM were collected, and their pathological, immunohistochemical, and molecular features were examined. A 1p/19q analysis via FISH, MGMT promoter methylation by MS-PCR, and IDH1 and BRAF V600E mutation analysis by HRM-PCR were performed. The level of EZH2 expression was valuated by immunohistochemistry in 15 E-GBM cases, and the prognostic factors were analyzed in E-GBM patients. Fifteen non-E-GBM cases were used as a control.
Results: The fifteen cases of E-GBM included twelve males and three females, with fourteen cases supratentorially located. Headache was the main symptom. Microscopy revealed that the tumors were composed of epithelioid cells and some rhabdoid cells. The epithelioid and rhabdoid cells displayed focal discohesion, scant intervening neuropil, a distinct cell membrane, eosinophilic cytoplasm, and a laterally positioned nucleus. Most tumors showed high mitosis, zonal necrosis, and microvascular hyperplasia. Immunohistochemical findings included epithelioid cells positive for GFAP, vimentin, nestin, S-100, and INI-1. The molecular findings included no deletions of 1p/19q, EGFR amplifications, or IDH1 mutations in any case, a methylated MGMT promoter in 46.7% (7/15) cases, and a BRAF V600E mutation in 46.7% (7/15) cases. EZH2 overexpression occurred in 60.0% (9/15) of E-GBM cases. E-GBM patients with OS (≤ 12 months) exhibited extensive necrosis (6/6), EZH2 overexpression (6/6), MGMT promoter unmethylation (5/6), BRAF V600E mutation (3/6), and treatment (surgery4/6). E-GBM patients with OS (> 12 months) exhibited focal or limited necrosis, low or negative EZH2 expression, MGMT promoter methylation (2/3), BRAF V600E mutation (3/3), and treatment (surgery+radiotherapy/chemo-radiotherapy, 2/3).
Conclusion: E-GBM was a rare variant of glioblastoma, with histological epithelioid features and poor prognosis. Extensive necrosis, MGMT promoter unmethylation, EZH2 overexpression, and lack of adjuvant chemo-radiotherapy may indicate a poor prognosis.
Keywords: central nervous system tumor, epithelioid glioblastoma, immunohistochemistry, clinicopathological features, molecular genetics, differential diagnosis