110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中性粒细胞与淋巴细胞比率的动态变化预测了经动脉化疗栓塞治疗的肝细胞癌患者的预后
Authors Wang H, Lin C, Fan W, Zhang J, Zhang Y, Yao W, Li J
Received 18 January 2020
Accepted for publication 21 April 2020
Published 14 May 2020 Volume 2020:12 Pages 3433—3444
DOI https://doi.org/10.2147/CMAR.S245396
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Seema Singh
Purpose: To examine the effect of dynamic changes in neutrophil-to-lymphocyte ratio (NLR) on tumor response and overall survival (OS) in patients with hepatocellular carcinoma (HCC) undergoing transarterial chemoembolization (TACE).
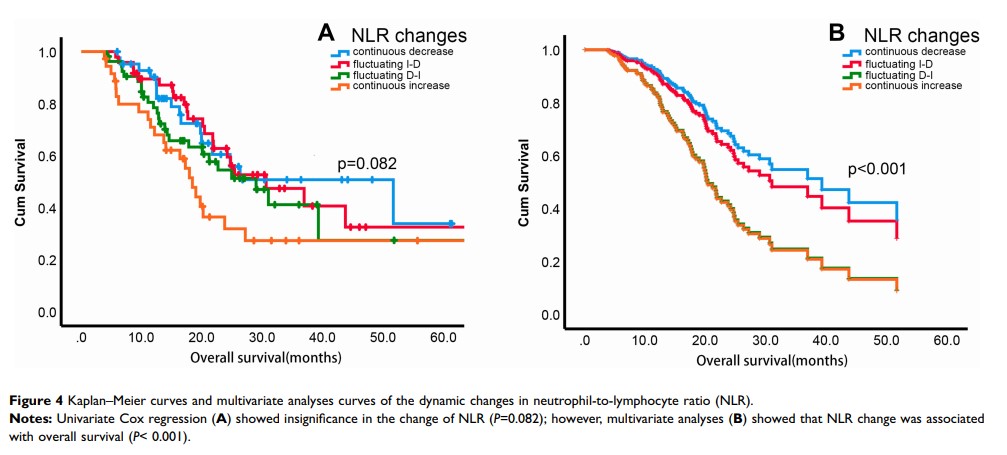
Patients and Methods: Data from 181 patients with HCC were retrospectively collected. White blood cell, neutrophil and lymphocyte counts, and the NLR were obtained 1– 3 days before as well as 3– 6 weeks and 3 months after TACE. Patients were divided into two groups at each time point according to the mean value of NLR, and also divided into continuous decrease, fluctuating increase-decrease (I-D), fluctuating decrease-increase (D-I), and continuous increase groups according to the dynamic changes in the NLR. The dynamic changes in blood counts and NLR were analyzed using repeated-measures ANOVA. The odds ratios (ORs) for tumor response in different NLR groups were examined using a multivariate logistic regression model. Finally, the prognostic value of the dynamic changes in the NLR was examined using Cox regression models.
Results: Continuous decline of white blood cell counts, neutrophil counts and lymphocyte counts were observed at 3– 6 weeks and 3 months after TACE treatment. The NLR increased slightly and then decreased substantially in responders, while it increased slightly and then significantly in non-responders, with a significant interaction effect of Time × Tumor response (P = 0.005). NLR grouping before TACE, 3– 6 weeks and 3 months after TACE was not associated with tumor response, and only 3 months after TACE did, it shows a significant difference in univariate survival analyses (NLR > 2.5 vs NLR ≤ 2.5, hazard ratio [HR] = 2.442, 95% confidence interval (CI): 1.545, 3.860). The changes in the NLR were significantly correlated with tumor response and OS. Non-responders for TACE were more common in the continuous NLR increase group (OR = 6.230, 95% CI: 1.848– 21.001) and in the fluctuating D-I group (OR = 5.702, 95% CI: 1.480– 21.957). Multivariate analyses revealed that these two patient groups also showed poorer OS (HR = 2.351, 95% CI: 1.120– 4.605 and HR = 2.320, 95% CI: 1.187– 4.533, respectively).
Conclusion: Dynamic changes in the NLR may be better predictors of tumor response and OS than static NLR values, but more data are needed.
Keywords: hepatocellular carcinoma, prognosis, neutrophil-to-lymphocyte ratio, transarterial chemoembolization