110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

由于重症监护病房中多药耐药的鲍曼不动杆菌,采用高剂量替加环素治疗老年肺炎患者
Authors Bai XR, Jiang DC, Yan SY
Received 11 February 2020
Accepted for publication 21 April 2020
Published 18 May 2020 Volume 2020:13 Pages 1447—1454
DOI https://doi.org/10.2147/IDR.S249352
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Purpose: The association between clinical and microbiological outcomes and high-dose tigecycline (TGC) was assessed in elderly (≥ 60 years old) patients with hospital-acquired and ventilator-associated pneumonia due to multidrug-resistant Acinetobacterbaumannii (A. baumannii ). This study also assessed tigecycline combination with different antibiotics and its influence on the outcome.
Patients and Methods: An observational retrospective cohort study was conducted. Patients over 60 years old were treated with standard-dose (SD) TGC (100-mg intravenous TGC initially, followed by 50-mg doses administered intravenously twice daily) and high-dose (HD) TGC (200-mg intravenous TGC initially, followed by 100-mg doses administered intravenously twice daily) for a microbially confirmed infection. The outcome was 30-day crude mortality, co-administered antimicrobial agent and the microbial eradication percentage in both groups.
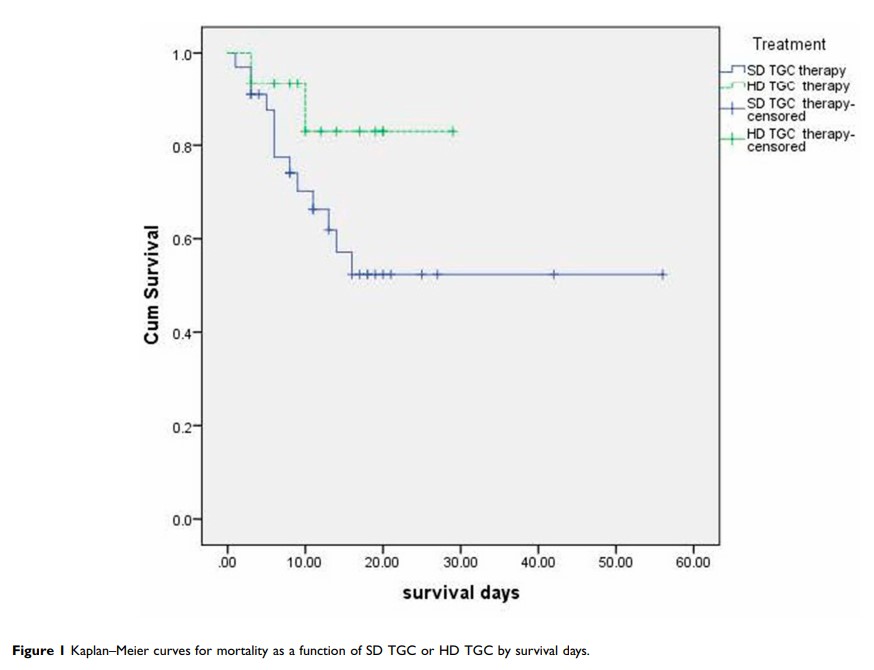
Results: A total of 48 multidrug-resistant A. baumannii respiratory patients were identified. Tigecycline was administered to 85% of ventilation-associated pneumonia (VAP) patients (28/33) in the SD group and 80% of VAP patients (12/15) in the HD group. Combined therapy was the major treatment option in both groups, accounting for 85% and 87%, respectively. Median treatment duration in both groups was 7.36 vs 8.6 days, respectively. Survival days were 13.61 vs 12.4 days (P =0.357), respectively. The 30-day crude mortality was 39.4% (13/33) for the SD group and 14% (2/15) for the HD group (P =0.098). The microbial eradication rate of respiratory specimens in the SD group was higher than that in the HD group (P =0.02). The variables associated with 30-day crude mortality were chronic obstructive pulmonary disease (hazard ratio [HR] 11.63, 95% CI 1.094– 123.058; P =0.042), tigecycline treatment duration (HR 0.690, 95% CI 0.515– 0.926; P =0.013), and surgery before infection (HR 79.276, 95% CI 6.983– 899.979; P =0.000). High-dose tigecycline was not associated with 30-day crude mortality (adjusted HR 0.329, 95% CI 0.074– 1.460; P =0.145). Combined antibiotics was also not different between the two groups.
Conclusions: High-dose tigecycline was not associated with 30-day crude mortality in elderly patients with pneumonia due to multidrug-resistant A. baumannii , although the microbial eradication rate was high.
Keywords: pneumonia, critical ill patients, high-dose tigecycline, drug-resistant, Acinetobacter baumannii