110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

鉴别继立体定向放射外科治疗后出现局部和远处复发且预后良好的脑转移患者
Authors Jiang X
Received 25 February 2020
Accepted for publication 13 May 2020
Published 3 June 2020 Volume 2020:12 Pages 4139—4149
DOI https://doi.org/10.2147/CMAR.S251285
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Sanjeev Srivastava
Purpose: This retrospective study aimed to determine the prognostic factors associated with overall survival after intracranial local and distant recurrence in patients undergoing stereotactic radiosurgery (SRS) for brain metastases.
Patients and Methods: Clinical characteristics and therapeutic parameters of 251 patients, who were treated with initial stereotactic radiosurgery for brain metastases and later experienced intracranial recurrence, were analyzed to identify prognostic factors of post-recurrence overall survival (PROS). A Cox proportional hazard model was applied for univariate and multivariate analyses.
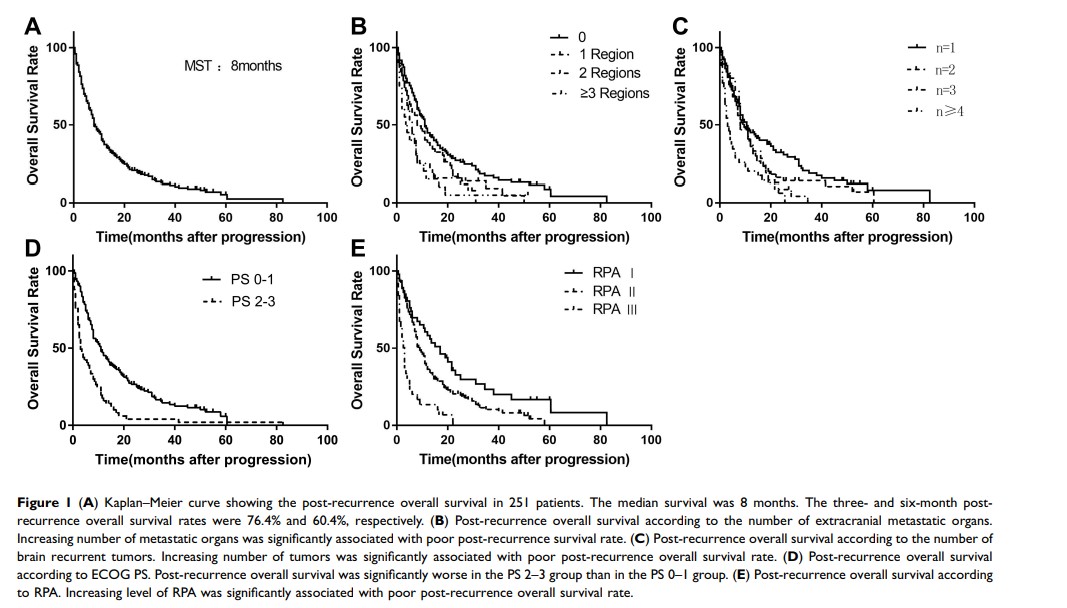
Results: Among the 251 patients, the median post-recurrence overall survival was 8 months, and the six-month PROS rate was 60.2%. The interval from initial radiosurgery treatment to intracranial recurrence (hazard ratio [HR]:0.970), the number of brain recurrent tumors (HR:1.245), the number of extracranial metastatic organs (HR:1.183), recursive partition analysis (RPA) (HR:1.778), and Eastern Cooperative Oncology Group Performance Status (ECOG PS) (HR:2.442) were identified as independent prognostic factors. The patients who received local treatment for solitary brain recurrence achieved better survival (the median survival time after recurrence was 22 months). In patients without extracranial metastasis, the median post-recurrence overall survival of the local treatment group was longer than that in the whole brain radiation therapy (WBRT) group (P < 0.001) and the systemic therapy group (P < 0.001).
Conclusion: A shorter interval from initial stereotactic radiosurgery to recurrence, an increasing number of brain recurrences and extracranial metastatic organs, and poor RPA and ECOG PS values are associated with poor post-recurrence prognosis. When the number of brain recurrent tumors and extracranial metastatic organs was limited, local treatment including stereotactic radiosurgery, surgery or intensity-modulated radiation therapy (IMRT) improved the post-recurrence overall survival.
Keywords: stereotactic radiosurgery, brain metastases, prognostic factors, intracranial recurrence, salvage treatment