110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

同种异体骨移植可重建下肢恶性骨肿瘤切除术后的大段骨干骨缺损
Authors Liu Q, He H, Duan Z, Zeng H, Yuan Y, Wang Z, Luo W
Received 15 April 2020
Accepted for publication 13 May 2020
Published 8 June 2020 Volume 2020:12 Pages 4299—4308
DOI https://doi.org/10.2147/CMAR.S257564
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Eileen O'Reilly
Aim: To evaluate the clinical effect of intercalary allograft transplantation and reconstruction in the treatment of diaphyseal defect after resection of lower extremity malignant bone tumor.
Methods: Clinical data of 17 patients diagnosed with malignant lower-limb bone tumors and having undergone segmental allograft reconstruction with a mean follow-up of 49.8 (26– 78) months were included. Segmental allografts of average 17-cm length preserved by deep-freezing were used and fixed using intramedullary nail, double plate, and intramedullary nail and plate combination in 2, 5, and 10 patients, respectively. Host–donor junctions were perfectly and roughly matched in 5 and 12 patients, respectively. Allograft union, local recurrence, and complications were assessed using clinical and radiological tests. Allograft union was evaluated using the International Society of Limb Salvage (ISOLS) scoring system. The functional prognosis was evaluated using the Musculoskeletal Tumour Society (MSTS) scoring system.
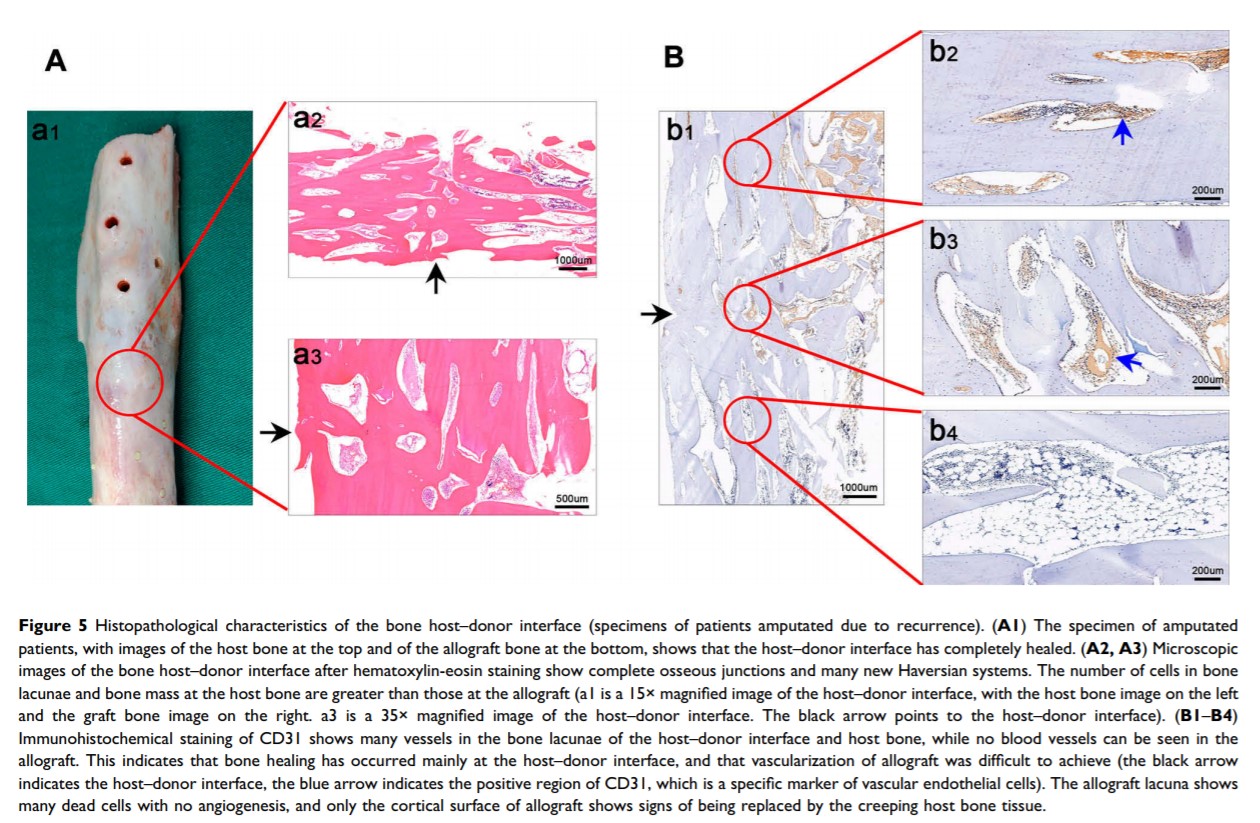
Results: Intercalary allograft reconstruction of femoral shaft, tibial shaft, and distal tibia with ankle arthrodesis was performed in eight, four, and five patients, respectively. Two patients had local recurrence and underwent amputation; one died of metastasis. Host–donor junctions in two patients showed nonunion; 12 patients achieved bone union. The average union time was 12.1 months. No allograft fracture or infection occurred. Union rates were 100% and 88.2% at metaphyseal and diaphyseal junctions, respectively. Healing time differed significantly between the precisely and roughly matched groups (p< 0.01). The incidence of nonunion was higher after intramedullary nailing than after the other two methods (p< 0.05). The mean MSTS score was 24.2 (14– 29) at the end of follow-up.
Conclusion: Intercalary allograft transplantation is an effective strategy for diaphyseal defect following post-tumor resection in the lower extremity. Good bone healing after allograft reconstruction is achieved with stable internal fixation and perfectly matched host–donor interfaces.
Keywords: intercalary allograft, malignant bone tumor, bone healing, lower extremity, internal fixation