110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国人群中万古霉素相关的急性肾损伤风险预测模型的推导和验证
Authors Xu N, Zhang Q, Wu G, Lv D, Zheng Y
Received 12 March 2020
Accepted for publication 25 May 2020
Published 22 June 2020 Volume 2020:16 Pages 539—550
DOI https://doi.org/10.2147/TCRM.S253587
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Background: Vancomycin is the standard therapy for methicillin-resistant Staphylococcus aureus (MRSA) infection; however, nephrotoxicity happened with a high incidence of 15%∼ 40%. Weighting the risk before receiving vancomycin treatment facilitates timely prevention of nephrotoxicity, but no standardized strategy exists for this purpose.
Methods: A retrospective cohort study was performed. A total of 524 hospitalized patients treated with vancomycin were included in this study. They were divided into derivation cohort (n=341) and externally validation cohort (n=183) according to their admission time. Using univariate and multivariable logistic regression, we identified potential predictors of vancomycin-associated acute kidney injury (AKI) and developed a risk score by plotting nomogram. The predictive performance of this novel risk score was assessed and validated by discrimination and calibration. Besides, the risk score was also compared with existing prediction models according to integrated discrimination index (IDI) and net reclassification index (NRI).
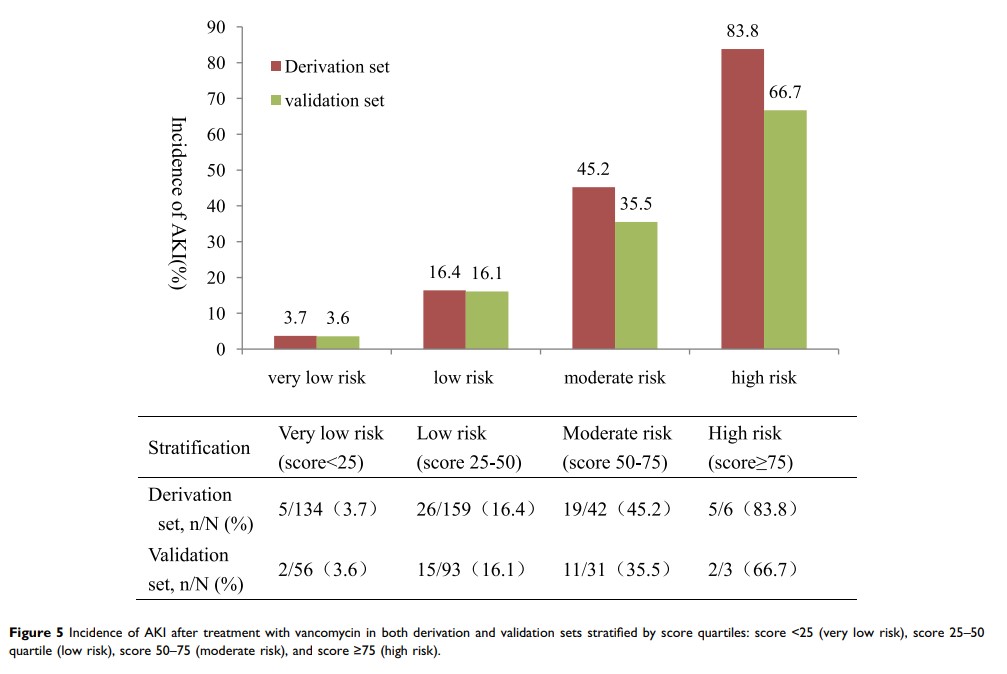
Results: The incidence of AKI was 16.1% (55/341) in the derivation cohort and 16.4% (30/183) in the validation cohort. Three factors (vancomycin serum trough concentration, piperacillin/tazobactam and furosemide) were determined as predictors for vancomycin-associated AKI. The established three-item risk score showed a comparable discrimination in both derivation cohort (AUC=0.793, 95% CI: 0.732– 0.855) and validation cohort (AUC=0.788, 95% CI: 0.698– 0.877). The risk score also demonstrated a good calibration in the derivation cohort (χ 2=6.079, P =0.638> 0.05) and validation cohort (χ2=5.665, P =0.686> 0.05). Compared with prediction by Cmin alone, this risk score significantly improved reclassification accuracy (IDI=0.050, 95% CI: 0.024– 0.076, P < 0.001, NRI=0.166, 95% CI: 0.044– 0.289, P=0.007).
Conclusion: The established model in this study is a simplified three-item risk score, which provides a robust tool for the prediction of AKI after receiving vancomycin treatment.
Keywords: vancomycin, acute kidney injury, prediction model