110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国农村社区曾患有妊娠期糖尿病的妇女糖耐量异常的进展及相关危险因素
Authors Mao P, Jiang S, Guo J, Jiang Y, Long Q, Tang Y, Luo J, Wiley J, Vorderstrasse A
Received 5 March 2020
Accepted for publication 8 June 2020
Published 29 June 2020 Volume 2020:13 Pages 2259—2268
DOI https://doi.org/10.2147/DMSO.S252542
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Background: The purpose of this study was to describe the status of abnormal glucose tolerance with a longer duration after delivery among women with prior gestational diabetes mellitus (GDM) in a rural community of China, and to explore the influence of socio-demographic factors, GDM-related factors (family history of diabetes, number of children, receipt of treatment for GDM), psychosocial factors (perceived stress, self-efficacy, and social support), lifestyle behaviors (physical activity, sedentary activity, fruit or vegetables intake), and obesity indicators (body mass index and waist circumferences) on abnormal glucose tolerance.
Patients and Methods: A cross-sectional descriptive survey was conducted among women with prior GDM in two county-level hospitals in Western and Eastern Hunan, China from November 2017 to June 2018. Under the guidance of life course theory, data were collected using self-report measures of socio-demographic and GDM-related factors as well as psychosocial factors (perceived stress, self-efficacy, and social support) and postpartum lifestyle behaviors (physical activity, sedentary activity, and fruit and vegetable intake). Additionally, a 75-g oral glucose tolerance test was conducted, and weight, height, and waist circumference were measured on site.
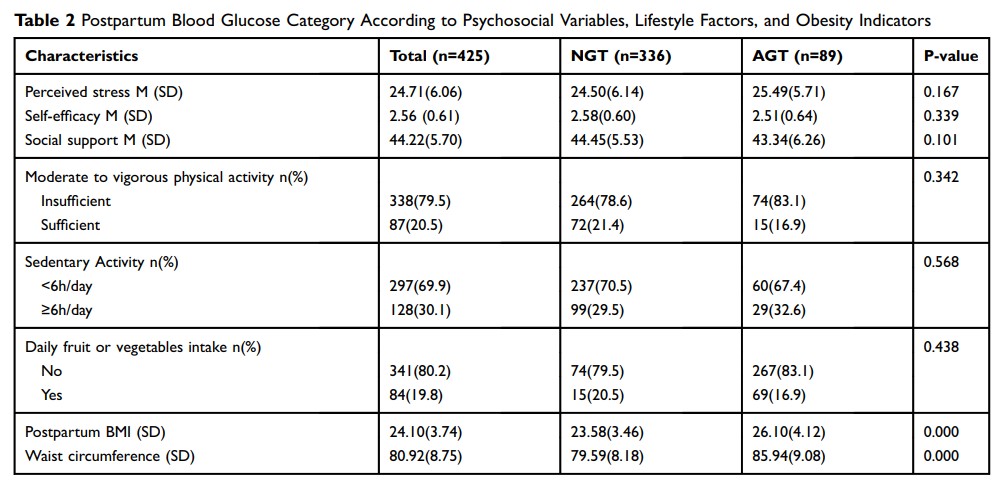
Results: A total of 425 women were included in this study, with an average postpartum duration of 18.04 months. Of these women, 20.9% had abnormal glucose tolerance (AGT). A multivariate analysis indicated that the proportion of abnormal glucose tolerance increased with increased age (OR = 2.13; 1.27– 3.57, p=0.004), ethnic minority (OR: 1.62, 95% CI: 0.96– 2.72, p=0.069), lower educational levels (OR:0.58, 95% CI: 0.33– 1.02, p=0.057), receipt of treatment for GDM during pregnancy (OR =1.93; 1.11– 3.37, p=0.020) and larger waist circumference (OR = 1.08; 1.05– 1.12, p=0.000).
Conclusion: More than one-fifth of the women with GDM in rural China had progression to AGT. More postpartum programs aimed at reducing waist circumference are warranted to delay or prevent progression to type 2 diabetes mellitus for rural Chinese women with prior GDM.
Keywords: gestational diabetes mellitus, abnormal glucose tolerance, postpartum, risk factors, waist circumference