110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

神经外科手术后患者的肠杆菌性脑膜炎/脑炎临床结果危险因素的纵向分析:2014-2019 年之间的一项比较队列研究
Authors Shi Y, Zheng G, Qian L, Qsman RA, Li G, Zhang G
Received 4 March 2020
Accepted for publication 17 June 2020
Published 6 July 2020 Volume 2020:13 Pages 2161—2170
DOI https://doi.org/10.2147/IDR.S252331
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Sahil Khanna
Purpose: Our study is a retrospective observational study conducted in one of the largest clinical centers of neurosurgery in China. We aimed to investigate the antimicrobial susceptibility patterns of the Enterobacteriaceae isolates responsible for nosocomial meningitis/encephalitis in post-neurosurgical patients. Meanwhile, we tried to evaluate the risk factors for mortality following Enterobacteriaceae meningitis/encephalitis.
Patients and Methods: Medical data on clinical characteristics, antibiotic susceptibilities, and mortality were reviewed until patients’ discharge or death in the hospital. Data for a total of 164 cerebrospinal fluid (CSF) infection cases due to Enterobacteriaceae after neurosurgery were collected between January 2014 and November 2019 in order to identify risk factors affecting the outcome. Kaplan–Meier survival analysis and multivariable Cox proportional hazard models were applied.
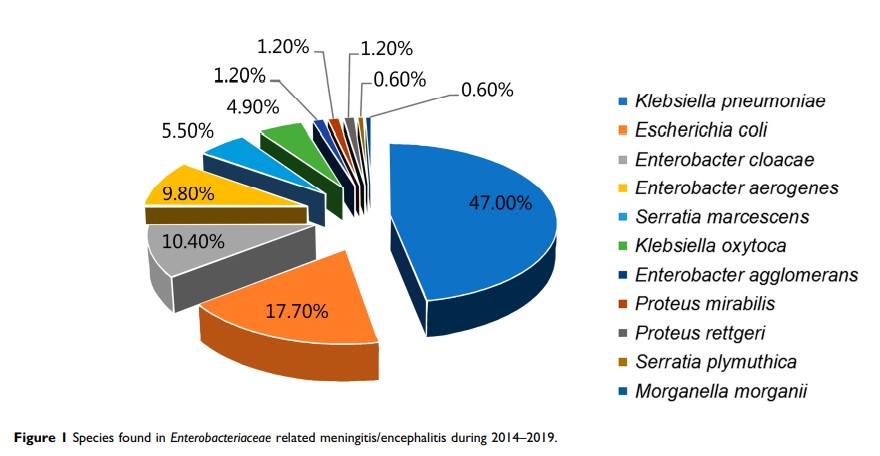
Results: In this study, a total of 2416 neurosurgical meningitis/encephalitis cases were reported between 2014 and 2019. Enterobacteriaceae accounted for 7.3% (176/2416) of all the bacterial infections. Of them, 164 Enterobacteriaceae isolates were available to divide into two groups according to the final outcome of whether the patient died or survived. In total, 38 patients died (23.2%) and 126 patients survived (76.8%). The most frequent infecting species was Klebsiella pneumoniae (47.0%, 77/164). Fourteen-day and 30-day mortality rates were 7.9% (13/164) and 15.2% (25/164). Kaplan–Meier survival analysis revealed that the risk factors of Enterobacteriaceae meningitis/encephalitis that resulted in poor outcomes included comorbidities, Glasgow Coma Scale (GCS) score, sepsis, intensive care unit (ICU) admission, extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae , and ventilation. A GCS score of less than or equal to 8 (P=0.04, HR 2.562) was identified to be a significant risk factor for mortality according to the multivariable Cox proportional hazards model.
Conclusion: In-hospital mortality caused by Enterobacteriaceae meningitis/encephalitis in neurosurgery was high. A GCS score of ≤ 8 was an independent risk factor for mortality following Enterobacteriaceae meningitis/encephalitis in post-neurosurgical patients.
Keywords: Enterobacteriaceae , post-neurosurgical meningitis/encephalitis, antibiotic susceptibility, antibiotic resistance, in-hospital mortality