110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中性粒细胞与淋巴细胞的比率对携带 EGFR 突变的非小细胞肺癌脑转移的临床预后价值
Authors Li H, Wang W, Yang X, Lian J, Zhang S, Cao J, Zhang X, Song X, Jia S, Xue R
Received 21 February 2020
Accepted for publication 26 June 2020
Published 12 July 2020 Volume 2020:12 Pages 5659—5665
DOI https://doi.org/10.2147/CMAR.S250688
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Sanjeev Srivastava
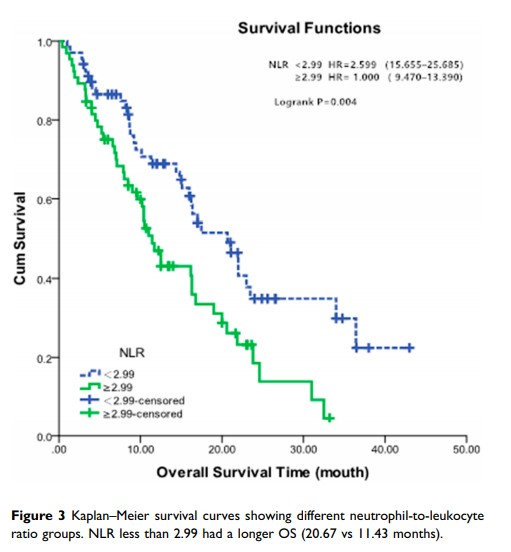
Purpose: Several studies have explored the correlation between the neutrophil-to-lymphocyte ratio (NLR) and the prognosis of patients with lung cancer. However, little is known about the correlation between the pretreatment NLR and the prognosis of patients with brain metastases from non–small cell lung cancer (NSCLC)-harboring mutations in the epidermal growth factor receptor (EGFR ) gene. We sought to evaluate the predictive values in brain metastasis from lung adenocarcinoma with EGFR mutations.
Methods: We retrospectively examined 133 patients with brain metastases (BMs) from lung adenocarcinoma with EGFR mutations. NLR was calculated using N/L, where N and L, respectively, refer to peripheral blood neutrophil (N) and lymphocyte (L) counts. The cut-off value of NLR was assessed by the area under the curve (AUC). The Log rank test and Cox proportional hazard model were used to confirm the impact of NLR and other variables on survival.
Results: An NLR value equal to or less than 2.99 was associated with prolonged survival in this cohort of patients in both variable and multivariable analysis.
Conclusion: We concluded that NLR is an independent prognostic factor in BMs from lung adenocarcinoma with EGFR mutations. This could serve as a useful prognostic biomarker and could be incorporated in the clinical prognostic index specific to patients with BMs.
Keywords: neutrophil-to-lymphocyte ratio, brain metastases, non–small cell lung cancer, EGFR mutations