110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

接受选择性胸腰椎融合手术的老年患者的虚弱状况和手术后结果
Authors Sun W, Lu S, Kong C, Li Z, Wang P, Zhang S
Received 9 January 2020
Accepted for publication 3 July 2020
Published 14 July 2020 Volume 2020:15 Pages 1141—1150
DOI https://doi.org/10.2147/CIA.S245419
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Background and Aim: Frailty is an independent predictor of mortality and adverse events (AEs) in patients undergoing surgery. This study aimed to quantify the ability of Modified Frailty Index (mFI) to predict AEs in older patients undergoing elective posterior thoracolumbar fusion surgery.
Methods: We retrospectively reviewed the results of 426 patients with the following diagnoses and follow-up evaluations of at least 12 months duration: lumbar disc herniation, 125; degenerative spondylolisthesis, 81; lumbar spinal canal stenosis, 187; and adult spinal deformities, 33. The cases were divided into two groups. The long spinal fusion (LSF) group was defined as ≥ 3 spinal levels with segmental pedicle-screw fixation. Short spinal fusion (SSF) were defined with at most two levels. The mFI used in the present study is an 11-variable assessment. The association of frailty with AEs was determined after adjusting for known and suspected confounders.
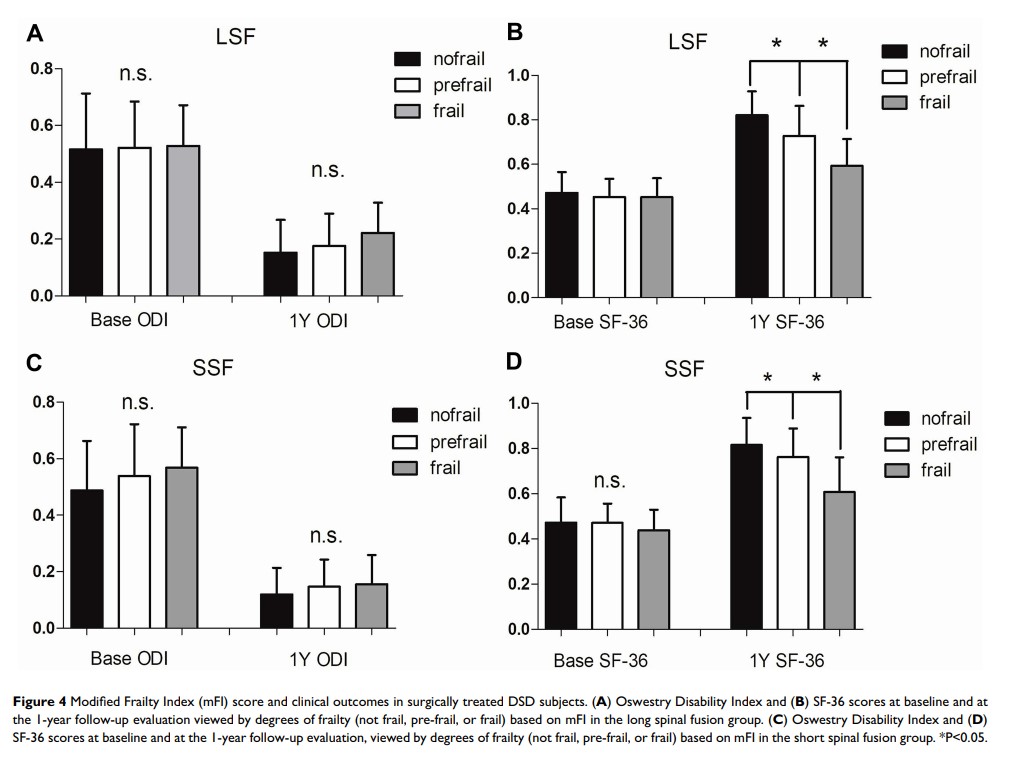
Results: Frailty was presented in 66 patients (15.5%) within the total population (LSF, 21.9% and SSF, 11.8%). Rates of AEs assessed in the study increased stepwise with an increase in the mFI for the two groups. The severity of frailty was an independent predictor of any, major, and minor complications in the LSF group and any, minor complication in the SSF group (P< 0.05). A comparison of post-operative clinical outcomes showed that the ODI and SF-36 scores deteriorated as the mFI increased.
Conclusion: Frailty was shown to be an independent predictor of AEs in older patients undergoing elective posterior thoracolumbar fusion surgery, especially for patients undergoing LSF.
Keywords: frailty, degenerative spine disease, spinal surgery, elderly, clinical evaluation, complications, risk stratification