108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

血小板计数升高可预测乳腺癌锁骨上淋巴结转移患者的不良预后
Authors Liu S, Fang J, Jiao D, Liu Z
Received 10 April 2020
Accepted for publication 8 July 2020
Published 20 July 2020 Volume 2020:12 Pages 6069—6075
DOI https://doi.org/10.2147/CMAR.S257727
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Background: More and more studies show that platelets are closely related to the occurrence and development of tumors. This study aims to explore the predictive value of peripheral blood platelet count on the prognosis of breast cancer patients with ipsilateral supraclavicular lymph node (ISLN) metastasis.
Methods: Eighty-five breast cancer patients with ISLN metastasis in the Affiliated Cancer Hospital of Zhengzhou University were collected retrospectively in this study. Chi-square test was used to analyze the correlation between clinical pathological data and platelet count. DFS rate was estimated by K-M curve and Log Rank test was performed. Univariate and multivariate Cox regression were used to determine the prognostic value of platelets. Time-dependent Cox regression was used to further analyze the correlation between peripheral blood platelets and prognosis to determine the stability of the results.
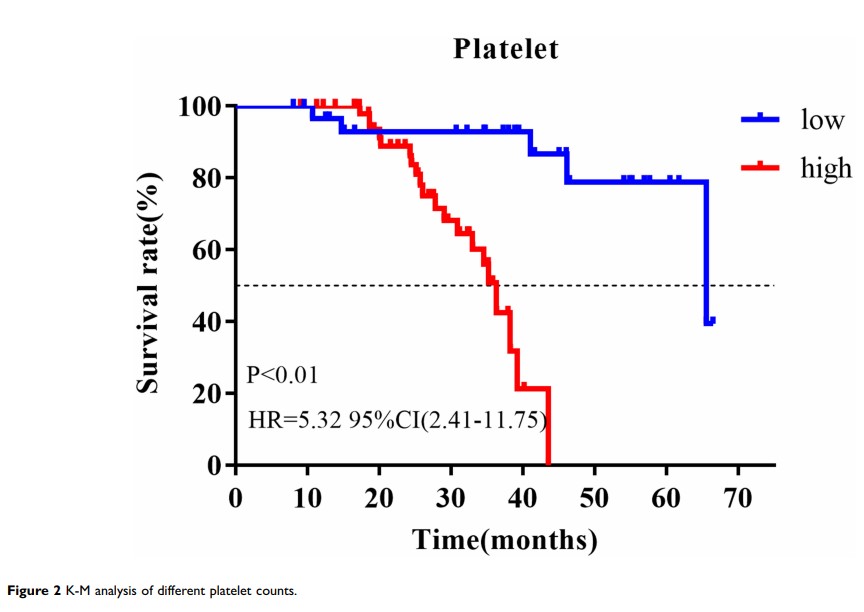
Results: The pathological complete response rate of ISLN after neoadjuvant chemotherapy (NAC) was 51.8%. Platelet count was correlated with PR status of breast cancer at first visit (P =0.01). After a median follow-up of 30 months, multivariate Cox analysis showed that high platelet count (HR=3.18, 95% CI=1.13– 8.93, P =0.028), premenopausal status (HR=0.40, 95% CI=0.17– 0.97, P =0.043), and ISLN pathological failure (HR=0.25 95%, CI=0.10– 0.62, P < 0.01) were associated with poor prognosis. K-M curve analysis showed that the prognosis of patients with a high platelet count was worse than that of patients with low platelet count (HR=5.32, 95% CI=2.41– 11.75, P < 0.01). To further verify the stability of this result, multivariate time-dependent Cox model also suggested that higher platelet level was related to poor prognosis (HR=1.009, 95% CI=1.003– 1.016, P < 0.01). Meanwhile, menopausal status (HR=0.32, 95% CI=0.14– 0.76, P =0.01) and sPCR (HR=0.29, 95% CI=0.12– 0.70, P =0.01) were also independent predictors of DFS.
Conclusion: Platelets have important predictive value for the prognosis of breast cancer patients with ISLN metastasis, which indicates that platelet count can be used to distinguish high-risk patients so as to obtain clinical benefits.
Keywords: platelet, neoadjuvant chemotherapy, prognosis, ipsilateral supraclavicular lymph nodes