108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

对于肝动脉介入治疗的肝细胞癌患者,炎症因子的预后价值:一项回顾性研究
Authors Guo L, Ren H, Pu L, Zhu X, Liu Y, Ma X
Received 12 April 2020
Accepted for publication 26 June 2020
Published 13 August 2020 Volume 2020:12 Pages 7173—7188
DOI https://doi.org/10.2147/CMAR.S257934
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chien-Feng Li
Background: Hepatic artery interventional therapy has been recognized as the first choice for advanced liver cancer. However, reliable prognostic markers are still lacking. In the present study, we aimed to evaluate the prognostic value of inflammation factors including neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR) and monocyte to lymphocyte ratio (MLR) in hepatocellular carcinoma (HCC) patients with hepatic artery interventional treatments.
Methods: Patients undergoing hepatic artery interventional therapy after being diagnosed with HCC between 2007 and 2014 were enrolled. Pre-treatment NLR, PLR and MLR were calculated, and all factors including gender, age, TNM stage, BCLC staging, inflammation factors, LDH, ALP, CEA, AFP, hepatitis, liver cirrhosis, portal vein involvement, surgical history and hepatic artery interventional treatment on overall survival (OS) were evaluated by the univariate and multivariate Cox proportional hazards analyses.
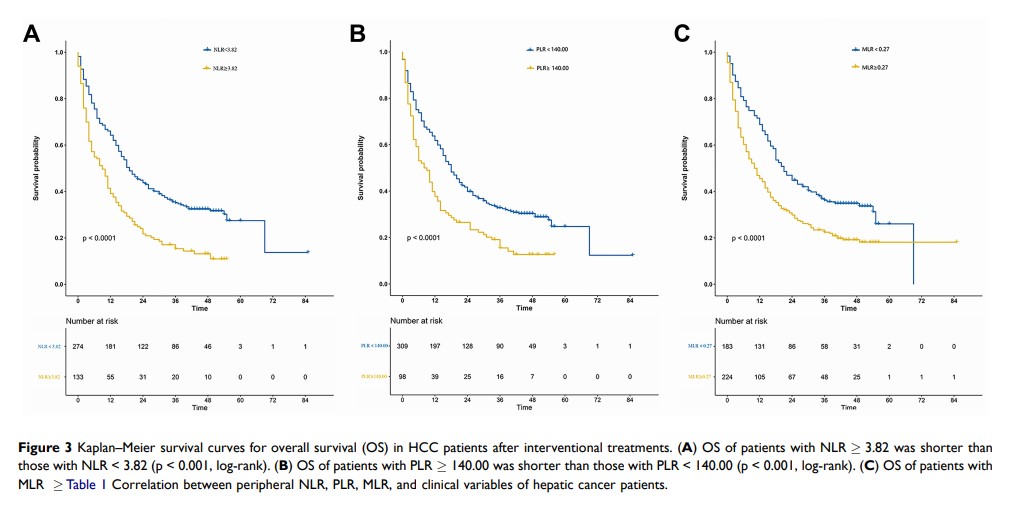
Results: Overall, 407 patients were included. The optimal cutoff values determined by receiver operating characteristic (ROC) curve analyses for NLR, PLR and MLR were 3.82, 140.00 and 0.27, respectively. High NLR was associated with worse OS (median survival time: high NLR group 9 vs low NLR group 19 months, HR 1.842, 95% CI: 1.457– 2.329, P< 0.001). Elevated PLR was negatively correlated with OS (8 vs 18 months, HR 1.677, 95% CI: 1.302– 2.161, P< 0.001). Patients in high MLR group had a worse OS (10 vs 21 months, HR 1.626, 95% CI: 1.291– 2.048, P< 0.001). In multivariate analysis, NLR, LDH, ALP and portal vein involvement were independent prognostic factors for OS of HCC patients after hepatic artery interventional therapy. In addition, for patients in BCLC stage A and B, higher NLR, PLR and MLR were all significantly negatively correlated to median survival time (NLR: 17 vs 26 months, HR: 1.739 (95% CI: 1.279– 2.365), P< 0.001; PLR: 18 vs 26 months, HR: 1.681 (95% CI: 1.245– 2.271), P=0.001; MLR: 20 vs 26 months, HR: 1.589 (95% CI: 1.185– 2.129), P=0.002).
Conclusion: Elevated pre-treatment NLR, PLR and MLR were associated with worse survival time in HCC patients after hepatic artery interventional therapy. Among them, NLR was an independent prognostic factor for OS.
Keywords: hepatocellular carcinoma, neutrophils, platelets, lymphocytes, inflammation, prognosis