108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

诺模图可预测接受新辅助放化疗的局部切除的晚期直肠癌患者的总体生存率
Authors Song J, Chen Z, Huang D, Wu Y, Lin Z, Chi P, Xu B
Received 17 April 2020
Accepted for publication 10 July 2020
Published 18 August 2020 Volume 2020:12 Pages 7375—7382
DOI https://doi.org/10.2147/CMAR.S255981
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Sanjeev Srivastava
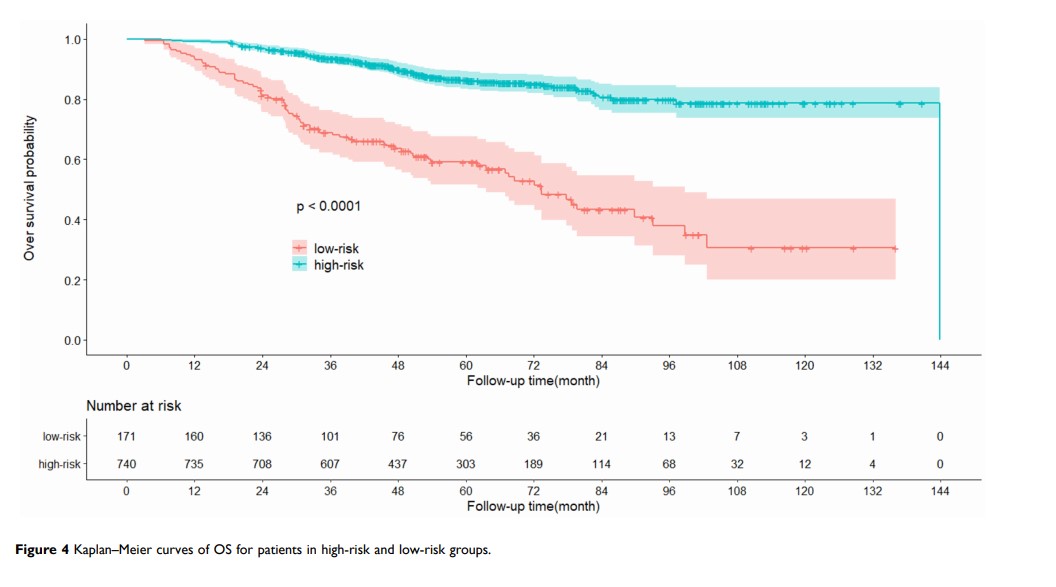
Purpose: The overall survival (OS) of resected locally advanced rectal cancer patients who underwent neoadjuvant chemoradiotherapy (nCRT) was significantly different, even among patients with the same tumor stage. The nomogram was designed to predict OS of rectal cancer with nCRT and divide the patients into different risk groups.
Materials and Methods: Based on materials from 911 rectal cancer patients with nCRT, the multivariable Cox regression model was carried out to select the significant prognostic factors for overall survival. And then, the nomogram was formulated using these independent prognostic factors. The discrimination of the nomogram was assessed by concordance index (C-index), calibration curves and time-dependent area under curve (AUC). The patients respective risk scores were calculated through the nomogram. The best cut-off risk score was calculated to stratify the patients. The survival curves of the two different risk cohorts were performed, which assessed the predictive ability of the nomogram.
Results: Age, cT stage, pretreatment CEA, pretreatment CA19-9, surgery, posttreatment CEA, posttreatment CA19-9, pT stage, pN stage and adjuvant chemotherapy were selected for the construction of the nomogram. And then the nomogram was constructed with independent prognostic factors. The C-index of the nomogram was 0.724, which showed the nomogram provided good discernment. The acceptable agreement between the predictions of nomogram and actual observations was illustrated by calibration plots for 3-, 5- and 10-year OS in the cohort. Time-dependent AUC with 6-fold cross-validation also showed consistent results of the nomogram. Risk group stratification confirmed that the nomogram had great capacity for distinguishing the prognosis.
Conclusion: The nomogram was developed and validated to predict overall survival of resected locally advanced rectal cancer patients with nCRT. The proposed nomogram might help clinicians to develop individualized treatment strategies. However, further studies are warranted to optimize the nomogram by finding out other unknown prognostic factors, and more external validation is still required.
Keywords: rectal cancer, nomogram, overall survival, neoadjuvant chemoradiotherapy