108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

影响小儿和成年皮细胞母细胞瘤患者治疗反应和总体生存率的不良因素
Authors Huo XL, Wang B, Zhang GJ, Ma JP, Wang L, Zhang LW, Xu XY, Li XJ, Li H, Li D, Zhang JT, Wu Z
Received 1 May 2020
Accepted for publication 30 July 2020
Published 18 August 2020 Volume 2020:12 Pages 7343—7351
DOI https://doi.org/10.2147/CMAR.S258476
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Eileen O'Reilly
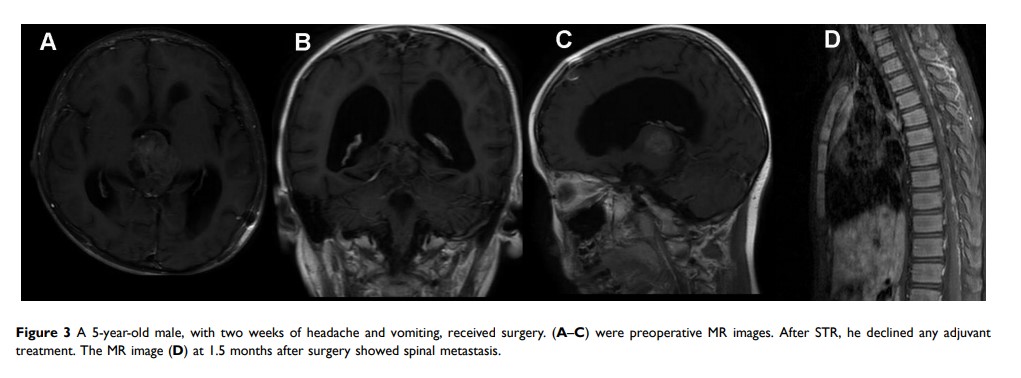
Objective: Intracranial pineoblastomas are rare neoplasms with poor prognosis. The aim of this study was to describe the independent prognostic factors and treatment strategies for overall survival in pediatric and adult patients.
Methods: Sixty-four patients were surgically treated between January 2012 and December 2018.
Results: The series included 37 (57.8%) males and 27 (42.2%) females. Gross total resection was achieved in 41 (64.1%) cases, and the 1-, 3-, and 5-year rates of overall survival were 86.3, 52.3, and 36.6%, respectively. In the pediatric group (n=42), 28 patients (66.7%) were male, with the median, and the mean age was 4 and 6.2± 4.7 years, respectively. After a median follow-up of 25.0 months, twenty-six patients (61.9%) died, and the 1-, 3-, and 5-year rates of overall survival were 84.9, 46.4, and 26.7%, respectively. Postoperative radiotherapy (p=0.058) and postoperative chemotherapy (p=0.183) had a positive influence on the increased overall survival. Meanwhile, postoperative radiotherapy combined with chemotherapy following surgery had a positive impact on overall survival (p=0.174, Log rank). In the adult group, the mean overall survival was 67.3± 9.3 months (range, 0.8– 95.3 months), and the 1-, 3-, and 5-year rates of overall survival were 89.5, 64.4, and 64.4%, respectively. In this group, no statistical association was observed between clinical factors and outcomes. However, patients who received postoperative radiotherapy (60.7 vs 57.6 month, mean survival; p=0.510, Log rank) or chemotherapy (63.0 vs 59.9 month, mean survival; p=0.404, Log rank) had better survival rates compared with those who declined.
Conclusion: In the pediatric group, surgery with postoperative radiotherapy and chemotherapy was a favorable factor for overall survival. In the adult group, a positive trend in overall survival was found when patients received radiation and/or chemotherapy following surgery.
Keywords: pediatric patients, adult patients, treatment strategy, overall survival