108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

来自河南省多重耐药的结核分枝杆菌的吡嗪酰胺耐药性和突变模式
Authors Shi J, Su R, Zheng D, Zhu Y, Ma X, Wang S, Li H, Sun D
Received 7 May 2020
Accepted for publication 28 July 2020
Published 20 August 2020 Volume 2020:13 Pages 2929—2941
DOI https://doi.org/10.2147/IDR.S260161
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Purpose: This study was designed to identify the phenotypic and genotypic characteristics of pyrazinamide (PZA) resistance among multidrug-resistant Mycobacterium tuberculosis (MDR-TB) from Henan and to evaluate the efficacy of pncA, rpsA , and panD mutations in predicting PZA resistance.
Materials and Methods: A total of 152 MDR strains were included in this study. The Bactec MGIT system was used to determine PZA susceptibility for all strains. The pncA, rpsA , and panD genes were sequenced to identify any mutations, and the sequences were then aligned with the sequence of standard strain H37Rv. Moreover, the correlations between PZA-resistant phenotypes and treatment outcomes were analysed.
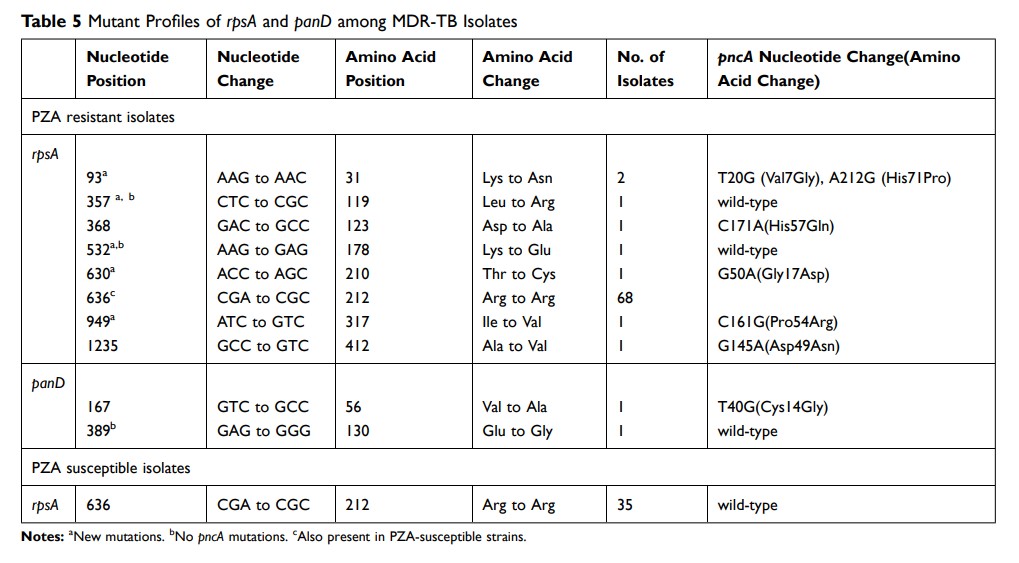
Results: Of the152 strains, 105 had a PZA-resistant phenotype, and 102 harboured the pncA mutation. The PZA resistance rate was higher in the strains with resistance to all four first-line drugs and those that were pre-extensively drug-resistant (pre-XDR) and extensively drug-resistant (XDR). A total of 100 different pncA mutation patterns were identified, including 80 point mutations and 20 insertions/deletions, and 32 new pncA mutation patterns were detected. In this study, 13 strains had multiple mutations. Of the11 PZA-resistant strains without pncA mutations, two harboured the rpsA mutation, and one harboured the panD mutation. With PZA susceptibility results as the reference, single-gene pncA sequencing had sensitivity of 89.52% and specificity of 89.36%. With the combination of rpsA and panD , the sensitivity increased to 92.38%, and the specificity remained the same. No significant differences were observed in the sputum smear/culture conversion rate between PZA-resistant patients and PZA-sensitive patients. However, PZA resistance was related to the time to sputum smear/culture conversion (P = 0.018).
Conclusion: The combination of pncA, rpsA , and panD was beneficial for the timely diagnosis of PZA resistance and could provide a laboratory basis for customizing treatment regimens for MDR-TB patients.
Keywords: Mycobacterium tuberculosis , multidrug-resistant, pyrazinamide, pncA , rpsA , panD