108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

手术联合放化疗对早期鼻咽癌近期和长期疗效的影响
Authors Weng JJ, Wei JZ, Li M, Zhang SJ, Wei YZ, Wang HW, Qin DX, Lu JL, Jiang H, Qu SH
Received 28 May 2020
Accepted for publication 7 August 2020
Published 25 August 2020 Volume 2020:12 Pages 7813—7826
DOI https://doi.org/10.2147/CMAR.S262567
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eileen O'Reilly
Objective: The efficacy of surgery as the primary treatment modality for nasopharyngeal carcinoma (NPC) is yet to be clarified. Therefore, we aimed to explore the short- and long-term efficacy of surgery for early-stage NPC.
Methods: We retrospectively evaluated 341 patients diagnosed with early-stage NPC between September 2010 and December 2015. Among them, 58 patients underwent endoscopic nasopharyngectomy combined with chemoradiotherapy, whereas 283 patients underwent conventional chemoradiotherapy. The patients who underwent concurrent chemoradiotherapy or radiotherapy alone were matched to patients who underwent surgery in a 1:2 ratio using propensity score matching to analyze the clinical efficacy of each therapeutic modality. The primary endpoint was survival, and the secondary endpoints were tumor regression rate and reduction in Epstein–Barr virus (EBV)-DNA levels.
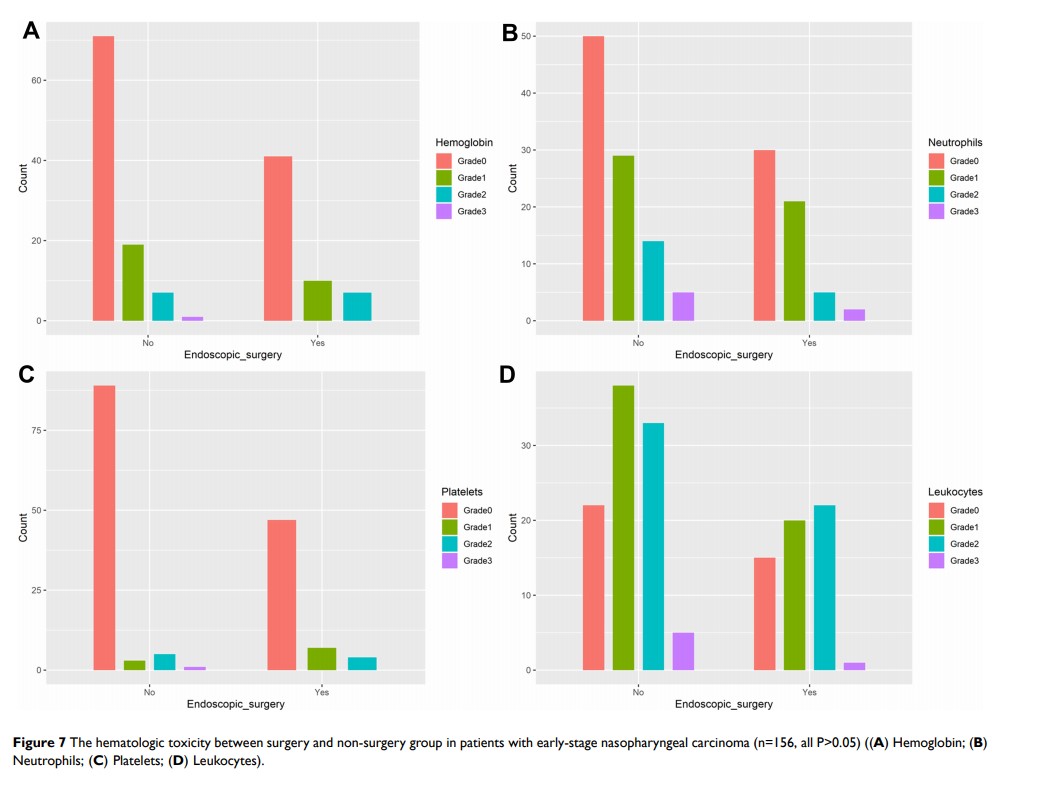
Results: After matching, 156 patients were enrolled (58 patients in the surgery group; 98 patients in the non-surgery group). The baseline data of the matched patients had good inter-group comparability (All P> 0.05). The surgery group had significantly higher 5-year overall survival (98.30% vs. 91.70%), disease-free survival (98.30% vs. 81.40%), and recurrence-free survival (100.00% vs. 90.10%) rates than did the non-surgery group (All P< 0.05). In total, 0 and 14 patients in the surgery and non-surgery groups, respectively, had residual cancer at the end of treatment (P=0.001). All patients in the surgery group tested negative for EBV-DNA, whereas two patients in the non-surgery group tested positive. The incidence of hematologic toxicity during treatment was similar between the two groups (All P> 0.05). Still, the incidence of severe oral mucositis was lower in the surgery group than in the non-surgery group (37.9% vs. 54.08%, P=0.051).
Conclusion: Surgery can improve the clearance rate of EB virus and reduce tumor residue. Surgery may be a safe and effective treatment for early NPC.
Keywords: nasopharyngeal carcinoma, endoscopic surgery, radiotherapy, prognosis