108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

SARS-CoV-2 和其他呼吸道病原体的合并感染
Authors Ma L, Wang W, Le Grange JM, Wang X, Du S, Li C, Wei J, Zhang JN
Received 11 June 2020
Accepted for publication 8 August 2020
Published 26 August 2020 Volume 2020:13 Pages 3045—3053
DOI https://doi.org/10.2147/IDR.S267238
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sahil Khanna
Purpose: To differentiate between respiratory infections caused by SARS-CoV-2 and other respiratory pathogens during the COVID-19 outbreak in Wuhan, we simultaneously tested for SARS-CoV-2 and pathogens associated with CAP to determine the incidence and impact of respiratory coinfections in COVID-19 patients.
Patients and Methods: We included 250 patients who were diagnosed with COVID-19. RT-PCR was used to detect influenza A, influenza B and respiratory syncytial viruses. Chemiluminescence immunoassays were used to detect IgM antibodies for adenovirus, Chlamydia pneumoniae and Mycoplasma pneumoniae in the serum of patients. Based on these results, we divided the patients into two groups, the simple SARS-CoV-2-infected group and the coinfected SARS-COV-2 group. Coinfected patients were then further categorized as having a coinfection of viral pathogen (CoIV) or coinfection of atypical bacterial pathogen (CoIaB).
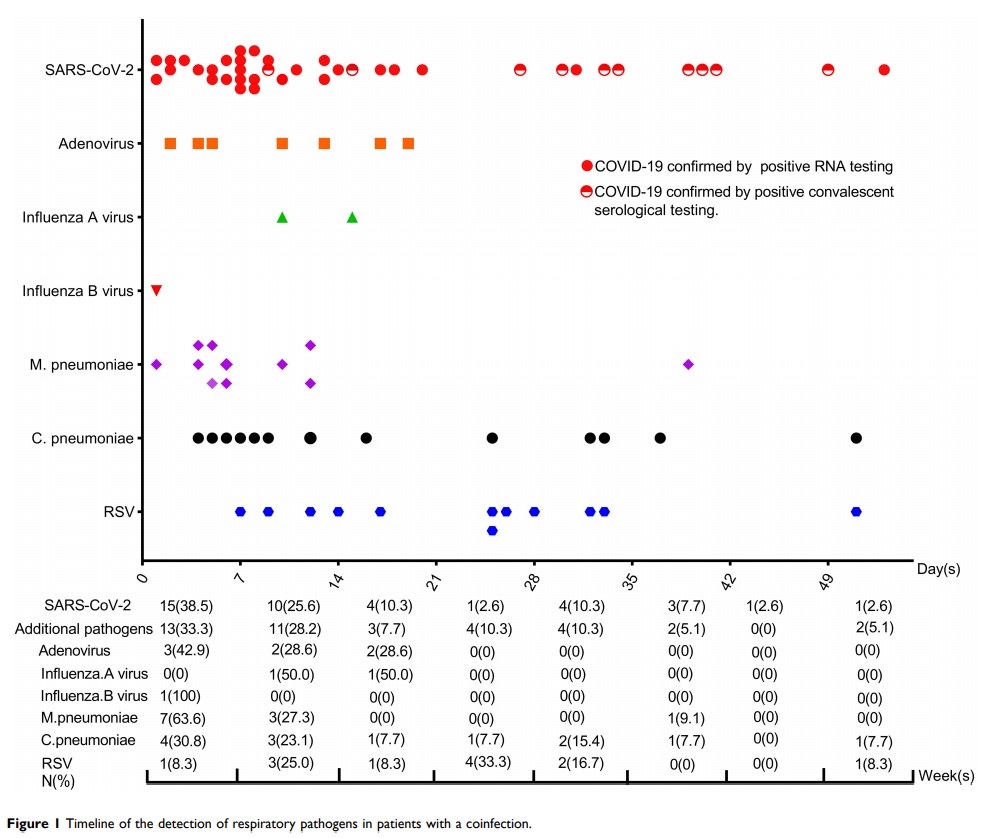
Results: No statistically significant differences were found in age, gender, the time taken to return negative SARS-CoV-2 nucleic acid test results, length of hospital stays, and mortality between the simple SARS-CoV-2 infection group and the coinfection group. Of the 250 hospitalized COVID-19 patients, 39 (15.6%) tested positive for at least one respiratory pathogen in addition to SARS-CoV-2. A third of these pathogens were detected as early as the 1st week after symptom onset and another third were identified after more than three weeks. The most detected CAP pathogen was C. pneumoniae (5.2%), followed by the respiratory syncytial virus (4.8%), M. pneumoniae (4.4%) and adenovirus (2.8%). Patients coinfected with viral pathogens (CoIV) (n=18) had longer hospital stays when compared to patients coinfected with atypical bacterial pathogens (CoIaB) (n=21). Except for one fatality, the remaining 38 coinfected patients all recovered with favourable outcomes.
Conclusion: Coinfections in COVID-19 patients are common. The coinfecting pathogens can be detected at variable intervals during COVID-19 disease course and remain an important consideration in targeted treatment strategies for COVID-19 patients.
Keywords: SARS-CoV-2, COVID-19, viral coinfection, atypical bacterial coinfection