108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

2017-2018 年在大型三级医院的无菌体液中分离出来的,产 NDM-5 的碳青霉烯类耐药的肺炎克雷伯菌 和产 SIM 的超病毒肺炎克雷伯菌 :使用 NGS 检测 bla NDM 样基因和 bla SIM 样基因的遗传特征
Authors Li Q, Zhu J, Kang J, Song Y, Yin D, Guo Q, Song J, Zhang Y, Wang S, Duan J
Received 11 May 2020
Accepted for publication 28 July 2020
Published 4 September 2020 Volume 2020:13 Pages 3075—3089
DOI https://doi.org/10.2147/IDR.S261117
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Purpose: To characterize the clinical, resistance, and virulence features of carbapenem-resistant Klebsiella pneumonaie (CRKP) and hypervirulent Klebsiella pneumoniae (hvKP) and also provide an effective selection of drug in CRKP and hvKP treatment.
Materials and Methods: Twelve strains were collected and investigated these isolates for their antimicrobial susceptibility and molecular features. Resistance mechanisms, virulence-associated genes, multilocus sequence typing (MLST), and serotypes were detected by PCR and sequencing. Next general sequencing (NGS) was carried out to determine the features of carbapenem resistance and virulence. The synergistic activity of tigecycline–imipenem (TGC+IPM), tigecycline–meropenem (TGC+MEM), and tigecycline–aztreonam (TGC+ATM) combinations were performed by microdilution checkerboard method.
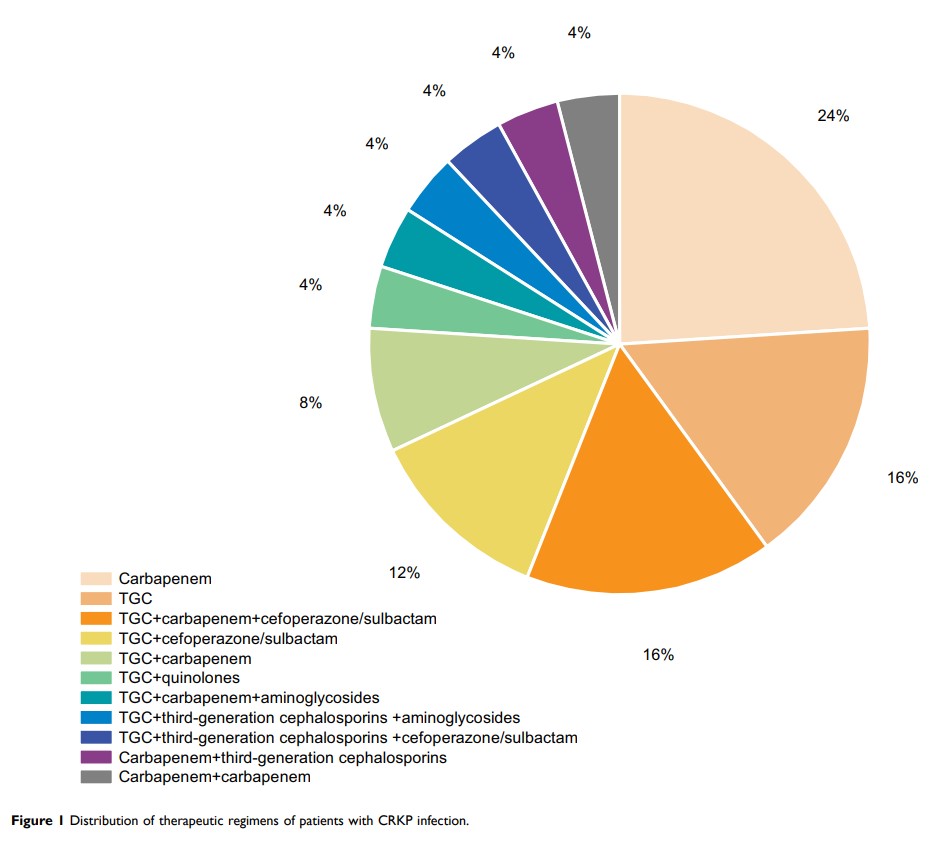
Results: Eleven CRKP and one hvKP strains were collected. All strains showed highly sensitive rates to tigecycline (TGC) and amikacin (AMK). NDM (33.3%, 4/12) was the main resistance mechanism and MLST assigned 3 of them to ST11. CTX-M-producing (n = 1) and KPC-2-producing (n = 1) isolates belonged to ST147 and ST11, respectively. The MICs of ATM and quinolones in NDM-1 CRKP and NDM-5 CRKP strains were different. The serotype of the majority strains was KL22KL137 (58.3%, 7/12), hvKP stain belonged to K64. CRKP strains harbored plasmid-mediated quinolone resistance genes (oqxA, oqxB, qnrS, qnrB), β-lactams (bla CTX-M-3), aminoglycosides, type I and type III fimbriae genes, siderophore genes, and transporter and pumps. SIM-producing ST1764 K64 showed typical features of hvKP, showing hypermucoviscosity phenotype. The virulence genes, including rmpA2, alls and aerobactin genes, linked to hvKP, were found in ST1764 hvKP. hvKP was sensitive to quinolone; also, oqxA gene was detected. All TGC combinations showed highly synergistic effects and TGC+IPM was more effective treatment.
Conclusion: We first identified the NDM-5-producing ST690 CRKP and SIM-producing ST1764 hvKP strains in Shanxi province. Tigecycline-carbapenem combinations were available treatments for CRKP.
Keywords: Klebsiella pneumoniae , hypermucoviscous, bla NDM-5, ST1764, tigecycline, synergistic effect