108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

预测不同大小、偶然发现的实性和亚实性肺结节的肺癌风险
Authors Zhang R, Tian P, Chen B, Zhou Y, Li W
Received 3 April 2020
Accepted for publication 13 August 2020
Published 4 September 2020 Volume 2020:12 Pages 8057—8066
DOI https://doi.org/10.2147/CMAR.S256719
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Beicheng Sun
Objective: Malignancy prediction models for pulmonary nodules are most accurate when used within nodules similar to those in which they were developed. This study was to establish models that respectively predict malignancy risk of incidental solid and subsolid pulmonary nodules of different size.
Materials and Methods: This retrospective study enrolled patients with 5– 30 mm pulmonary nodules who had a histopathologic diagnosis of benign or malignant. The median time to lung cancer diagnosis was 25 days. Four training/validation datasets were assembled based on nodule texture and size: subsolid nodules (SSNs) ≤ 15 mm, SSNs between 15 and 30 mm, solid nodules ≤ 15 mm and those between 15 and 30 mm. Univariate logistic regression was used to identify potential predictors, and multivariate analysis was used to build four models.
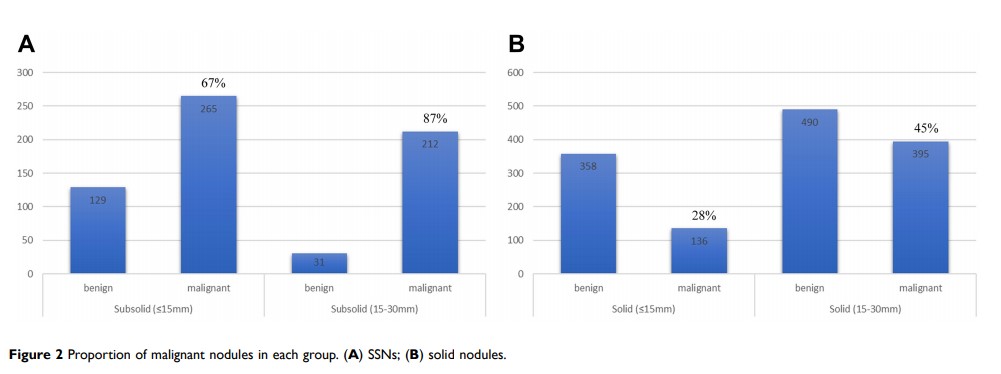
Results: The study identified 1008 benign and 1813 malignant nodules from a single hospital, and by random selection 1008 malignant nodules were enrolled for further analysis. There was a much higher malignancy rate among SSNs than solid nodules (rate, 75% vs 39%, P < 0.001). Four distinguishing models were respectively developed and the areas under the curve (AUC) in training sets and validation sets were 0.83 (0.78– 0.88) and 0.70 (0.61– 0.80) for SSNs ≤ 15 mm, 0.84 (0.74– 0.93) and 0.72 (0.57– 0.87) for SSNs between 15 and 30 mm, 0.82 (0.77– 0.87) and 0.71 (0.61– 0.80) for solid nodules ≤ 15 mm, 0.82 (0.79– 0.85) and 0.81 (0.76– 0.86) for solid nodules between 15 and 30 mm. Each model showed good calibration and potential clinical applications. Different independent predictors were identified for solid nodules and SSNs of different size.
Conclusion: We developed four models to help characterize subsolid and solid pulmonary nodules of different sizes. The established models may provide decision-making information for thoracic radiologists and clinicians.
Keywords: lung cancer, subsolid nodule, solid nodule, prediction model