108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

术前纤维蛋白原-白蛋白比率指数(FARI)是新辅助放化疗治疗后接受根治性手术的局部晚期直肠癌患者可靠的预后和放化疗敏感性预测因子
Authors Lu S, Liu Z, Zhou X, Wang B, Li F, Ma Y, Wang W, Ma J, Wang Y, Wang H, Fu W
Received 22 July 2020
Accepted for publication 29 August 2020
Published 17 September 2020 Volume 2020:12 Pages 8555—8568
DOI https://doi.org/10.2147/CMAR.S273065
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eileen O'Reilly
Background: Inflammatory response and nutritional status are associated with cancer development and progression. The purpose of this study was to explore whether the preoperative fibrinogen-albumin ratio index (FARI) is related to prognosis and chemoradiotherapy outcome of radical surgery after neoadjuvant chemoradiotherapy (NCRT) in patients with locally advanced rectal cancer (LARC).
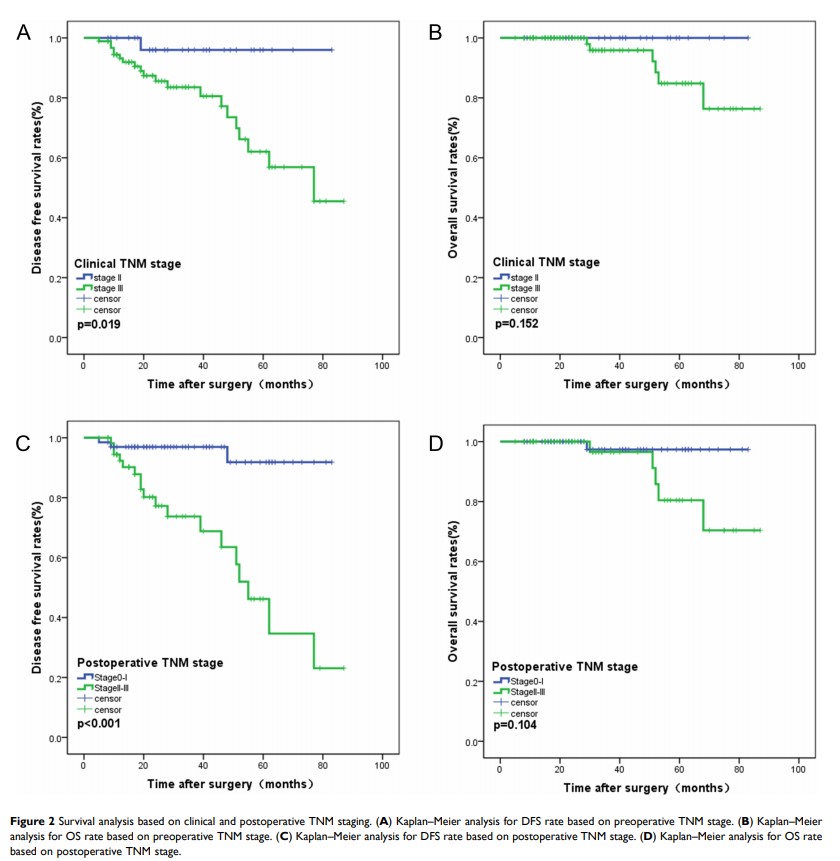
Methods: In total, 123 patients with LARC who underwent radical surgery after NCRT between June 2012 and December 2018 were collected in this study. Time-dependent receiver operating characteristic (ROC) curve analysis was made to evaluate the ability of the markers for forecasting prognosis. The correlation between FARI and clinicopathological parameters was analyzed. The Kaplan–Meier survival analysis, univariate and multivariate analysis based on Cox proportional hazards models, and subgroup analysis were performed to evaluate overall survival (OS) and disease-free survival (DFS). A nomogram was constructed to evaluate the predictive role of FARI in DFS.
Results: The ROC curve analysis showed that the ability of FARI on DFS prediction was superior to those of other inflammatory markers and carcinoembryonic antigen (CEA) (P< 0.05). Based on the Youden’s index, the optimal cut-off value of FARI was 8.8%. High FARI patients (> 8.8%) showed a poor response to NCRT and a decreased DFS rate (P< 0.05). In addition, multivariate analysis revealed that FARI (HR=3.098, P=0.033), neutrophil-to-lymphocyte ratio (NLR), and postoperative T stage were independent prognostic factors for DFS in TNM stage III LARC patients. However, FARI failed to distinguish patients with poor OS. Harrell’s concordance index (C-index) of the nomogram containing FARI (0.807) was obviously higher than that without it (0.732) among LARC patients who underwent radical surgery after NCRT. Moreover, multivariate analysis revealed FARI (OR=3.044, P=0.012) as an independent predictor for response to NCRT.
Conclusion: Among LARC patients who underwent radical surgery after NCRT, preoperative FARI is an independent prognostic factor for DFS and an independent predictor for response to NCRT.
Keywords: rectal cancer, fibrinogen-albumin ratio index, prognosis, tumor regression grade