108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

前列腺癌合并骨转移瘤患者接受细胞减少性前列腺切除术和转移灶导向放疗相结合疗法的肿瘤学结果:一项回顾性队列研究
Authors Xue P, Wu Z, Wang K, Gao G, Min Z, Yan M
Received 8 July 2020
Accepted for publication 4 September 2020
Published 23 September 2020 Volume 2020:12 Pages 8867—8873
DOI https://doi.org/10.2147/CMAR.S270882
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev Srivastava
Background: The current standard of care for metastatic prostate cancer (mPCa) is androgen deprivation therapy (ADT) with or without anti-androgen and chemotherapy. The aim of this study was to evaluate the efficacy and safety of a multimodal approach including local primary tumor therapy, metastasis-directed therapy (MDT), and hormonal therapy in patients with oligometastatic prostate cancer (PCa).
Methods: We reviewed data of patients with PCa and bone oligometastases at diagnosis treated in three institutions with ADT followed by cytoreductive surgery with or without metastases-directed radiotherapy. Oligometastases were defined as the presence of five or fewer metastatic lesions with the absence of visceral metastases. In this retrospective cohort study, 58 patients underwent cytoreductive radical prostatectomy and ADT. Of these, 26 patients (45%) received stereotactic body radiation therapy (SBRT) to all metastatic sites as a MDT. Oncological outcomes were analyzed using the Kaplan–Meier method.
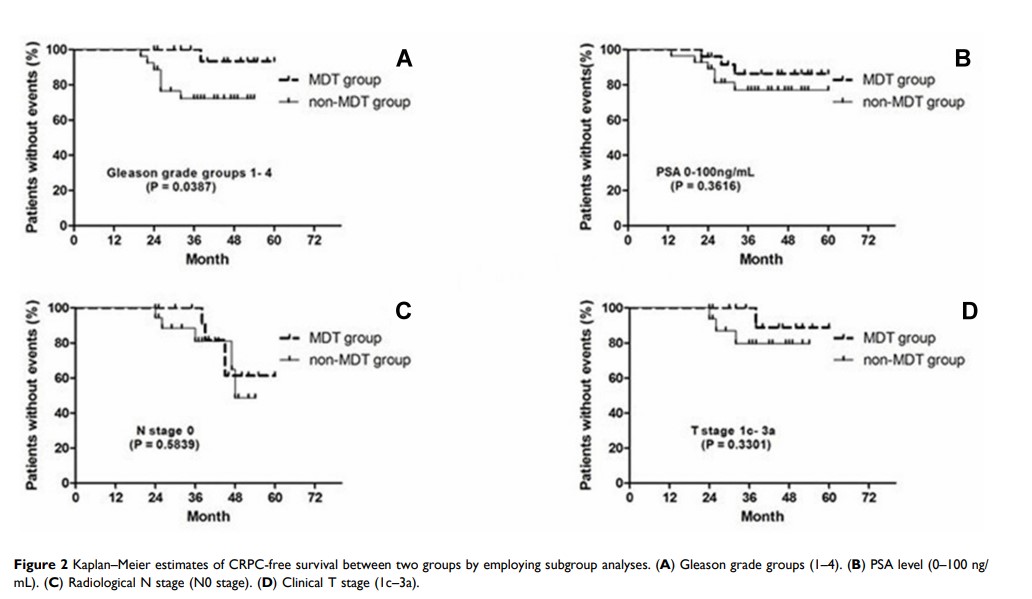
Results: The median follow-up period was 46.2 months. Of the 58 patients, the 3-year castration-resistant prostate cancer (CRPC)-free survival and cancer-specific survival was 75.9% and 91.4%, respectively. Pre- or post-treatment predictive factors for progression to CRPC, including prostate-specific antigen (PSA) level at diagnosis ≥ 20 ng/mL, Gleason grade groups 5, clinical T stage cT3b-4, PSA nadir level of ≥ 0.05 ng/mL, and no MDT with SBRT, were significantly associated with progression to CRPC. Subgroup analysis showed that the MDT group had significantly better CRPC-free survival than the non-MDT group with Gleason grade groups 1– 4 (HR=0.228; 95% CI= 0.056– 0.926). A total of 3.4% of the patients had grade 2 acute genitourinary toxicities and 5.2% had grade 2 acute gastrointestinal toxicities. No late grade > 2 adverse events were observed.
Conclusion: This multi-center, retrospective cohort study revealed the feasibility of combining cytoreductive prostatectomy and metastasis-directed radiotherapy for newly-diagnosed oligometastatic PCa. This treatment strategy has the potential to delay the progression to CRPC.
Keywords: oligometastases, prostate cancer, stereotactic body radiotherapy, androgen deprivation therapy, radical prostatectomy, metastasis-directed therapy