108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

评估 p16INK4a 免疫细胞化学在宫颈癌筛查中的表现
Authors Song F, Du H, Xiao A, Wang C, Huang X, Yan P, Liu Z, Qu X, Belinson JL, Wu R
Received 22 July 2020
Accepted for publication 1 September 2020
Published 25 September 2020 Volume 2020:12 Pages 9067—9075
DOI https://doi.org/10.2147/CMAR.S273079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev Srivastava
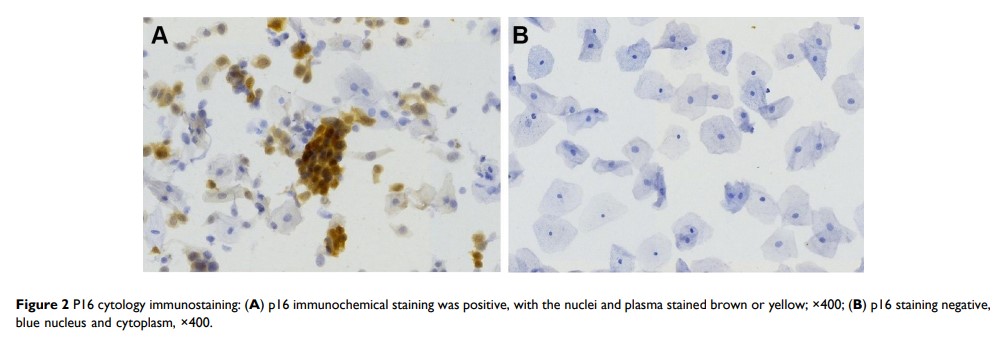
Purpose: When used for cervical cancer primary screening, liquid-based cytology (LBC) has a high specificity but a low sensitivity. For histological diagnosis of high-grade lesions, p16INK4a immunostaining has proven to be useful. Therefore, our objective was to evaluate the use of p16INK4a immuno-cytology as a primary screen and a secondary screen after primary high-risk human papillomavirus (hrHPV) screening or LBC screening.
Methods: A total of 1197 cytology slides were immuno-stained using automatic p16INK4a staining system (PathCIN®p16INK4a) in two studies from cervical screening programs. In the primary screening study, 875 slides were randomly selected and analyzed for p16INK4a. In the secondary screening study, 322 of the remaining slides were chosen by virtue of being HPV 16/18+, other hrHPV+/LBC≥ASC-US, or HPV-negative/LBC ≥LSIL. The sensitivity and specificity for detection of cervical intraepithelial neoplasia 2/3 or worse (CIN2+/CIN3+) were compared based on p16INK4a, LBC and HPV test results.
Results: In combining two studies, there were 431 cases with biopsy pathology. They included 83 cases with CIN2+ and 41 cases with CIN3+. The p16 positivity rate increased with pathologic and cytologic severity (P< 0.0001). For primary screening: p16 immuno-cytology was more specific than HPV testing and was similar in sensitivity. Also, p16 immuno-cytology compared favorably with routine LBC (≥ASC-US or ≥LSIL) in sensitivity and specificity. For secondary screening: after LBC screening, “Triaging ASC-US with p16” gave a higher specificity and a similar sensitivity as compared to the “Triaging ASC-US with hrHPV” algorithm. After HPV primary screening, p16 immuno-cytology was more specific than LBC (≥ASC-US); the calculated colposcopy referral rate was also decreased by using p16 immuno-cytology as triage. Triage of “HPV16/18 and p16” had higher specificity and similar sensitivity as compared to triage of “HPV16/18 and LBC ≥ASC-US”.
Conclusion: For primary screening, p16INK4a immuno-cytology compares favorably to routine LBC and HPV testing. p16INK4a immunostaining could be an efficient triage to reduce the colposcopy referral rate after primary hrHPV screening or LBC screening. Therefore, p16INK4a immuno-cytology may be applicable as a favorable technology for cervical cancer screening.
Keywords: cervical intraepithelial neoplasia, human papillomavirus, p16, immunochemical staining, cervical cancer screening