108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

采用下一代测序对切除边缘的致癌突变进行分子分析,从而预测非小细胞肺癌患者的复发
Authors Wei W, Li X, Song M, Wang C
Received 13 April 2020
Accepted for publication 2 September 2020
Published 25 September 2020 Volume 2020:13 Pages 9525—9531
DOI https://doi.org/10.2147/OTT.S257991
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Federico Perche
Objective: To investigate the genetic mutations in both tumor and marginal tissues in patients with non-small cell lung cancer (NSCLC), and to evaluate the potential prognostic value in patients with margins gene positive.
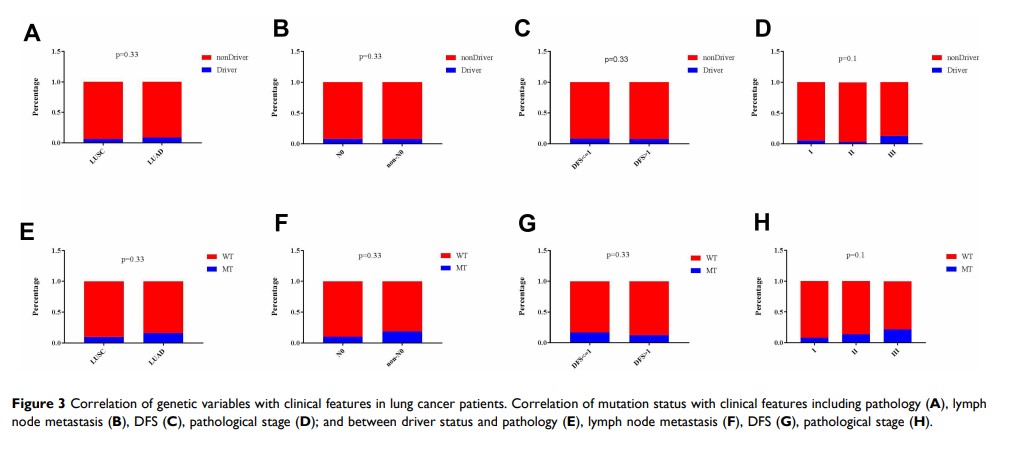
Methods: Next-generation sequencing (NGS) technique was used to detect genetic mutation in tumor and marginal tissues of the bronchus in 88 patients with NSCLC. Correlation of genetic mutations with pathology, lymph node metastasis, disease-free survival and overall survival was analyzed.
Results: Of the 88 patients, 83 cases (94.3%) had gene mutations in the tumor samples and 12 cases (13.6%) had genetic alterations in their margins. Most of the gene mutations detected were cancer drivers. Six common driver genes between tumor and marginal tissues were identified, including EGFR , TP53 , CDKN2A , CTNNB1 , BRAF , and NF1 . Kaplan–Meier analysis revealed that the median disease-free survival (DFS) was significantly shorter in patients with detectable gene mutations in marginal tissues compared with patients without mutations in margins (30.7 versus 24.4 months, log-rank χ 2 = 4.78, P =0.029). Consistently, a shorter median OS was observed in patients harboring gene mutations in margins compared with patients with no mutations in margins (49.1 versus 32.2 months, log-rank χ 2 = 3.669, P =0.055).
Conclusion: These findings identify the presence of oncogenic alterations in microscopically negative margins in NSCLC patients associated with elevated risk of relapse and shorter survival time. Thus, examination of microscopically negative margins by NGS represents a valuable approach to predict the clinical outcome of NSCLC patients.
Keywords: lung cancer, gene mutation, surgical margin, next-generation sequencing