108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

COPD 对应激性心肌病患者住院治疗效果的影响
Authors Li P, Lu X, Teng C, Cai P, Kranis M, Dai Q, Wang B
Received 11 June 2020
Accepted for publication 31 August 2020
Published 29 September 2020 Volume 2020:15 Pages 2333—2341
DOI https://doi.org/10.2147/COPD.S267289
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Purpose: Chronic obstructive pulmonary disease (COPD) is a known comorbidity of takotsubo cardiomyopathy (TCM), and COPD exacerbation is a potential triggering factor of TCM. The association between COPD and in-hospital outcomes and complications among TCM patients is not well established. We sought to assess the effect of COPD on hospitalized patients with a primary diagnosis of TCM.
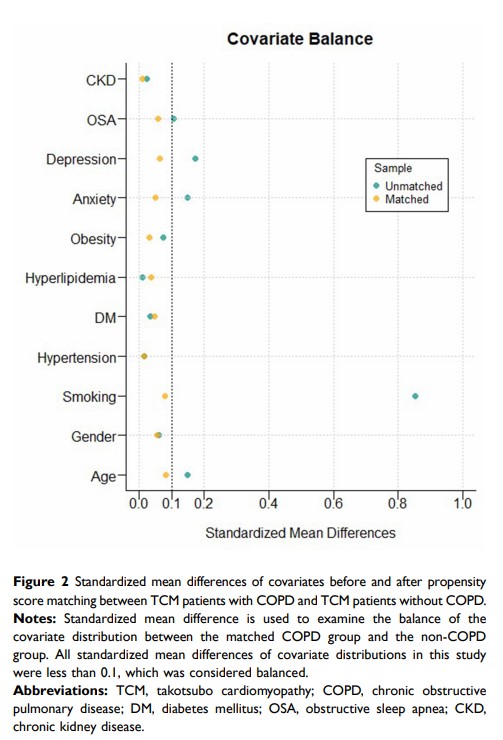
Methods: We conducted a retrospective cohort study in patients with a primary diagnosis of TCM with or without COPD using the latest National Inpatient Sample from 2016– 2017. We identified 3139 patients admitted with a primary diagnosis of TCM by the ICD-10-CM coding system; 684 of those patients also had a diagnosis of COPD. We performed propensity score matching in a 1:2 ratio (n=678 patients, matched COPD group; n=1070, matched non-COPD group) and compared in-hospital outcomes and complications between TCM patients with and without a COPD diagnosis.
Results: Before matching, the COPD group had worse outcomes compared with the non-COPD group in inpatient death (2.9% vs 1.3%, p=0.006), length of stay (LOS) (4.02± 2.99 days vs 3.27± 3.39 days, p< 0.001), hospitalization charges ($55,242.68± 47,637.40 vs $48,316.97± 47,939.84, p=0.001), and acute respiratory failure (ARF) (22.5% vs 7.7%, p< 0.001), respectively. After propensity score matching, the matched COPD group, compared with the matched non-COPD group, had a higher inpatient mortality rate (2.9% vs1.0%, p=0.005), longer LOS (4.02± 3.00 days vs 3.40± 3.54 days, p< 0.001), higher hospitalization charges ($55,409.23± 47,809.13 vs $46,469.60± 42,209.10, p< 0.001), and a higher incidence of ARF (22.6% vs 8.2%, p< 0.001) and cardiogenic shock (5.6% vs 3.3%, p=0.024), respectively.
Conclusion: Patients with COPD who are hospitalized for TCM have higher rates of inpatient mortality, ARF, cardiogenic shock, as well as a longer LOS, and higher charges of stay than those without COPD. Prospective studies are warranted to examine the effect of early intervention or treatment of COPD on short- and long-term outcomes of TCM.
Keywords: takotsubo cardiomyopathy, chronic obstructive pulmonary disease, in-hospital outcomes