110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

癌干细胞标志物 CD117 的过表达可预测上皮性卵巢癌患者预后不良: 综合分析所产生的证据
Authors Yang B, Yan X, Liu L, Jiang C, Hou S
Received 9 March 2017
Accepted for publication 25 April 2017
Published 13 June 2017 Volume 2017:10 Pages 2951—2961
DOI https://doi.org/10.2147/OTT.S136549
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr XuYu Yang
Purpose: Cancer stem cells have recently been identified as a key driving factor
for tumor metastasis and chemoresistance. CD117 is a well-established cancer
stem cell marker, but its clinical significance in epithelial ovarian cancer
(EOC) remains controversial. Therefore, we aimed to identify correlations
between CD117 expression and clinical features and outcomes in EOC patients in
this meta-analysis.
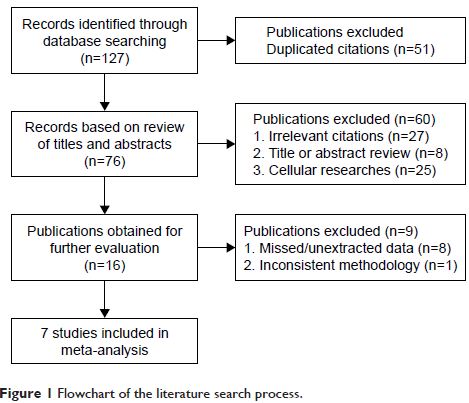
Materials and
methods: A literature search was performed in the PubMed, Cochrane Library, Web
of Science, EMBASE, and OVID databases to identify eligible studies.
Correlations between CD117 expression and clinicopathological parameters and
overall survival or disease-free survival were analyzed. A subgroup analysis
was then performed, which was classified by patient ethnicity and age at
diagnosis, study sample size, and tumor histological type.
Results: A total of seven studies enrolling 1,247 EOC patients were included in
this meta-analysis. Our results demonstrated that CD117 expression was
significantly correlated with age (pooled odds ratio [OR] =1.67, 95% confidence
interval [CI] =1.05–2.66), International Federation of Gynecology and
Obstetrics stage (pooled OR =1.99, 95% CI =1.31–3.02), tumor differentiation
grade (pooled OR =2.46, 95% CI =1.48–4.10), and histological type (pooled OR
=1.85, 95% CI =1.05–3.26). EOC patients with high CD117 expression had significantly
worse OS (hazard ratio [HR] =1.39, 95% CI =1.03–1.90) than patients with low
CD117 expression. However, no significant correlation was found between CD117
expression and disease-free survival (HR =1.31, 95% CI =0.79–2.17). In subgroup
analysis, CD117 was identified as a significant prognostic factor for overall
survival in European patients (HR =1.59, 95% CI =1.13–2.23), younger
patients (<60 years) (HR =1.59, 95% CI =1.10–2.30), studies with sample
sizes >200 (HR =1.84, 95% CI =1.32–2.56), and the mixed histological types
(HR =1.47; 95% CI =1.08–2.00).
Conclusion: Our meta-analysis suggests that CD117 is associated with EOC progression
and can serve as a promising prognostic predictor for EOC patients. However,
larger scale multicenter clinical trials are still needed to further validate
our results.
Keywords: epithelial ovarian cancer, CD117, cancer stem cell, prognosis