110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中性粒细胞淋巴细胞比率,以及血小板与淋巴细胞比值对 AECOPD 患者的预后评价和院内死亡率的预测
Authors Yao CY, Liu XL, Tang Z
Received 14 May 2017
Accepted for publication 1 July 2017
Published 3 August 2017 Volume 2017:12 Pages 2285—2290
DOI https://doi.org/10.2147/COPD.S141760
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Charles Downs
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Background and
objectives: Acute exacerbation of chronic
obstructive pulmonary disease (AECOPD) is one of the leading causes of hospitalization
and is associated with considerable mortality, for which clinicians are seeking
useful and easily obtained biomarkers for prognostic evaluation. This study
aimed to determine the potential role of the neutrophil–lymphocyte ratio (NLR)
and platelet–lymphocyte ratio (PLR) as prognostic makers for hospital mortality
in patients with AECOPD.
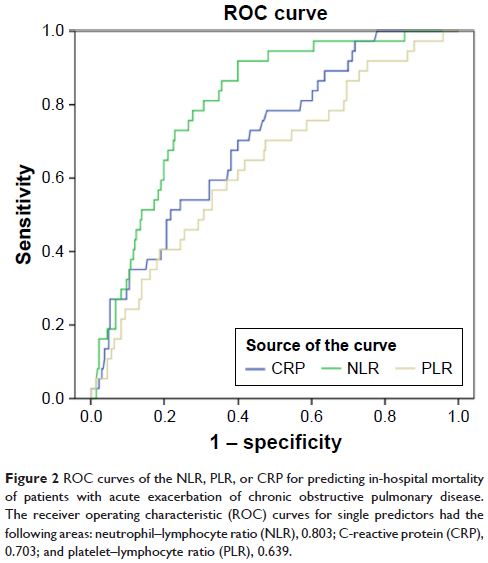
Methods: We included 303 patients with AECOPD in this
retrospective study. Clinical characteristics, NLR, PLR, and serum levels of
C-reactive protein (CRP) and other data were collected. Relationships between
NLR/PLR and CRP were evaluated by Pearson’s correlation test. Receiver
operating characteristics curve and the area under the curve (AUC) were used to
assess the ability of NLR and PLR to predict hospital mortality in patients
with AECOPD.
Results: Mean levels of NLR and PLR of all patients with AECOPD
were 7.92±8.79 and 207.21±148.47, respectively. NLR levels correlated with
serum CRP levels (r =0.281, P <0.05). The overall hospital
mortality rate was 12.21% (37/303). Levels of NLR and PLR were significantly
higher among non-survivors compared to survivors of AECOPD (both P <0.05). At a cut-off value of
6.24, the sensitivity and specificity of the NLR in predicting hospital
mortality were 81.08% and 69.17%, respectively, with an AUC of 0.803. At a
cut-off of 182.68, the corresponding sensitivity, specificity and AUC of PLR
were 64.86%, 58.27%, and 0.639. The combination of NLR, PLR, and CRP increased
the prognostic sensitivity.
Conclusion: NLR and PLR levels were increased in non-survivor
patients with AECOPD, and the NLR may be simple and useful prognostic marker
for hospital mortality in patients with AECOPD. More studies should be carried
out to confirm our findings.
Keywords: acute
exacerbation of chronic obstructive pulmonary disease, neutrophil–lymphocyte
ratio, platelet–lymphocyte ratio, hospital mortality, prognosis