110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

单核细胞与淋巴细胞比值预测接受新辅助化疗晚期胃癌患者的生存率
Authors Chen L, Hao Y, Zhu LH, Li S, Zuo YJ, Zhang YX, Song HJ, Xue YW
Received 21 April 2017
Accepted for publication 22 June 2017
Published 10 August 2017 Volume 2017:10 Pages 4007—4016
DOI https://doi.org/10.2147/OTT.S140118
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 2
Editor who approved publication: Dr Ingrid Espinoza
Background: Currently, precise predictors in gastric cancer patients
undergoing neoadjuvant chemotherapy are lacking. The study aims to investigate
the prognostic value of the monocyte to lymphocyte ratio (MLR) in patients with
advanced gastric cancer receiving S-1 plus oxaliplatin (SOX) or oxaliplatin and
capecitabine (XELOX) neoadjuvant chemotherapy regimen.
Methods: The data from Harbin Medical University Cancer Hospital from
August 2008 to September 2015 were retrospectively collected. Ninety-one
patients with advanced gastric cancer treated with neoadjuvant chemotherapy
were included. The blood samples were collected before neoadjuvant
chemotherapy. The MLR was divided into two groups: Low-MLR <0.27 group
and high-MLR ≥0.27 group. Survival curves were performed using the Kaplan–Meier
method and compared using the log-rank test. Univariate and multivariate Cox
proportional hazards regression model were evaluated to determine independent
prognostic factors.
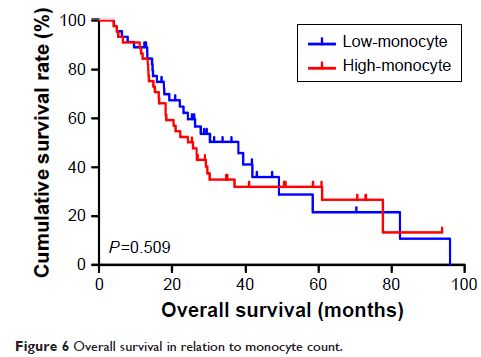
Results: The univariate analysis showed that median disease free survival (DFS)
and overall survival (OS) for all patients were better in low-MLR value group
than high-MLR value group (median DFS 26.80 and 23.73 months, P =0.653, respectively; median OS
27.93 and 26.87 months, P =0.807,
respectively). Multivariate analysis showed that MLR level was not an
independent prognostic factor of DFS and OS. Nevertheless, median DFS and OS
for all patients were better for patients with low monocyte values compared to
those with high monocyte values (median DFS 30.23 and 21.03 months, P =0.645, respectively; median OS
37.97 and 25.83 months, P =0.509,
respectively); in patients with high lymphocyte values compared with low
lymphocyte values median DFS was 26.87 and 21.03 months, (P =0.624) respectively; median OS
was 27.93 and 26.37 months, (P =0.584)
respectively. However, the patients with low level MLR had better 5-year DFS
and OS rates.
Conclusion: MLR may be used as a convenient and cheap prognostic marker in
patients with advanced gastric cancer undergoing neoadjuvant chemotherapy with
SOX or XELOX. Low level MLR as a prognostic marker may help doctors in terms of
efficient measures to treat gastric cancer.
Keywords: neoadjuvant chemotherapy, advanced gastric cancer, monocyte to
lymphocyte ratio (MLR), disease free survival, overall survival